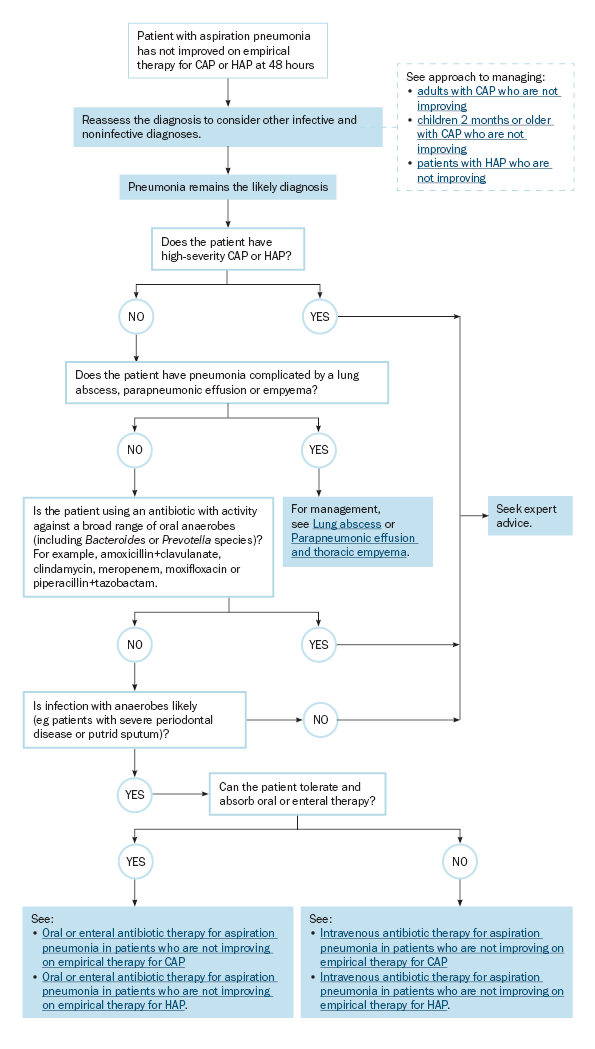
Management of aspiration pneumonia in patients who are not improving on empirical therapy for CAP or HAP
Management of aspiration pneumonia in patients who are not improving on empirical therapy for CAP or HAP outlines management of aspiration pneumonia in patients who are not improving on empirical therapy for community-acquired pneumonia (CAP) or hospital-acquired pneumonia (HAP).
Initial therapy for aspiration pneumonia is the same as empirical therapy for CAP or HAP, which treats most pathogens aspirated from the oropharynx, including oral anaerobes. If the response to empirical therapy is inadequate at 48 hours, reassess the diagnosis before adjusting the antibiotic regimen; consider other infective and noninfective diagnoses. For advice, see:
- Approach to managing adults with CAP who are not improving
- Approach to managing children 2 months or older with CAP who are not improving
- Approach to managing patients with HAP who are not improving.
In rare cases, pneumonia following aspiration may be due to specific anaerobes such as Bacteroides or Prevotella species that are not adequately treated with some empirical regimens for CAP or HAP. These pathogens are more likely in patients who have severe periodontal disease or putrid sputum. Assess for complications in patients with pneumonia involving anaerobic pathogens because it can be necrotising or cavitary, and may progress to lung abscess, parapneumonic effusion or empyema.
Anaerobic pathogens are difficult to detect using sputum samples but may be identified by blood culture or culture of lower respiratory tract samples. If an anaerobic pathogen is identified by culture, the infection is often polymicrobial, so monotherapy for anaerobic pathogens (eg metronidazole monotherapy) is not appropriate.
For management of patients with high-severity pneumonia who are not improving, seek expert advice.
CAP = community-acquired pneumonia; HAP = hospital-acquired pneumonia
