Resuscitation of patients with sepsis or septic shock
These guidelines include limited advice on resuscitation; consult local protocols or other references for comprehensive advice on nonantibiotic management of patients with sepsis or septic shock. For specific advice on resuscitation of neonates, infants or children with sepsis, refer to local protocols or seek expert advice.
Begin initial resuscitation with rapid assessment of the patient’s clinical state. This may require concurrent intervention with lifesaving resuscitation using an ABC (airway, breathing, circulation) approach.
Start management within 1 hour of presentation to medical care or, for ward-based patients, development of suspected sepsis or septic shock. Initial management includes:
- measuring blood lactate concentration12. If initial lactate concentration is more than 2 mmol/L, measure again within 2 to 4 hours to monitor effectiveness of resuscitation
- obtaining blood samples for culture1. Collect 2 sets (ie 4 bottles) from adults; a single smaller volume sample is appropriate for neonates and young children
- collecting other relevant samples as soon as possible, but not if doing so will delay antibiotic administration. Samples taken after antibiotic therapy has started can still be useful
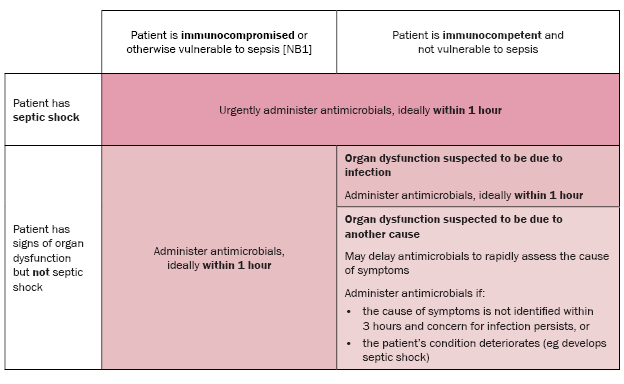
- administering broad-spectrum antibiotics3. Urgent administration of antibiotics, ideally within 1 hour of presentation to hospital or, for ward-based patients, development of suspected sepsis, is essential if:
- the patient has septic shock
- the patient is considered most vulnerable to sepsis
- the organ dysfunction is suspected to be due to infection
- beginning rapid administration of intravenous fluids to manage hypotension or a blood lactate concentration more than 2 mmol/L. If the patient is hypotensive during or after fluid resuscitation, give a vasopressor to maintain a mean arterial blood pressure of at least 65 mmHg4.
If a source of infection is identified, rapid specific treatment is essential (eg drainage of an abscess, removal of a vascular access device). Such management should be in consultation with appropriate specialist teams, because a timely multidisciplinary approach to sepsis management is associated with improved outcomes.
For immunocompetent patients without septic shock who are less vulnerable to sepsis, if there is less certainty that the organ dysfunction is due to infection, it is reasonable to defer antimicrobials to rapidly assess the cause of symptoms. If, however, the cause of symptoms is not identified within 3 hours of recognition and concern for infection persists, antimicrobials should be administered. Antimicrobials should be administered as soon as possible if the patient’s condition deteriorates during the assessment, or they develop septic shock.
For patients who are immunocompromised or otherwise vulnerable to sepsis, the risk of sepsis is significantly higher. These patients should receive antimicrobials within 1 hour of recognition, regardless of whether they have septic shock or the certainty that organ dysfunction is due to infection.
It is important to establish whether an advance care plan is in place and whether therapy for sepsis and septic shock is consistent with the expressed goals of the patient.
Australian Commission on Safety and Quality in Health Care (ACSQHC), 2022Evans, 2021
NB1: Patients who are most vulnerable to sepsis include very young and older people; Aboriginal and Torres Strait Islander peoples; patients who have recently had an invasive procedure or surgery; and patients with immune compromise (including those with autoimmune conditions, primary immunodeficiency or asplenia; taking immunosuppressant drug [eg high-dose corticosteroids]; and on long-term haemodialysis or peritoneal dialysis). For more information, see Patients who are most vulnerable to sepsis.
