Classification of coronary ischaemic syndromes
Patients with coronary ischaemic syndromes are classified by the pattern of their presenting symptoms; see Classification of coronary ischaemic syndromes.
Patients with new or increasing symptoms are classified as having an acute coronary syndrome, whereas those with chronic symptoms are classified as having stable angina. This distinction is important because an accelerated or new pattern of symptoms indicates the need for reassessment and treatment.
Acute coronary syndromes result from unstable atherosclerotic plaques or endothelial disruption, with associated transient or permanent thrombotic occlusion of the coronary arteries. This leads to myocardial ischaemia and infarction. Stable angina is usually due to a relatively fixed coronary obstruction produced by stable atherosclerotic plaque.
Based on the presence or absence of ST elevation on initial electrocardiogram (ECG), patients with an acute coronary syndrome are further subdivided into having:
- ST elevation myocardial infarction (STEMI)—a medical emergency
- non–ST elevation acute coronary syndrome (NSTEACS)—the initial description for patients without ST elevation. Subsequent investigation divides NSTEACS into:
- non–ST elevation myocardial infarction (NSTEMI)—patients with myocardial infarction as determined by elevated cardiac biomarkers
- unstable angina—patients without elevated cardiac biomarkers.
NSTEACS can progress to STEMI; ongoing monitoring is essential.
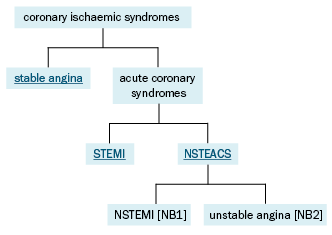
NSTEACS = non–ST elevation acute coronary syndrome; NSTEMI = non–ST elevation myocardial infarction; STEMI = ST elevation myocardial infarction
NB1: NSTEMI can progress to STEMI.
NB2: Unstable angina can progress to NSTEMI.
The fourth universal definition of myocardial infarction1 classifies myocardial infarctions into various types, which are managed differentlyThygesen, 2018.
In Type 1 myocardial infarction, atherothrombotic coronary occlusion (most commonly secondary to coronary plaque disruption [eg rupture or erosion]) compromises myocardial blood flow. Criteria for Type 1 myocardial infarction include detection of a rise and/or fall of cardiac troponin values with at least one value above the 99th percentile of the upper limit of normal and with at least one of the following:
- symptoms of acute myocardial ischaemia
- new ischaemic ECG changes
- development of pathological Q waves
- imaging evidence of new loss of viable myocardium or new regional wall motion abnormality in a pattern consistent with an ischaemic aetiology
- identification of a coronary thrombus by angiography including intracoronary imaging or by autopsy.
Management of Type 1 myocardial infarction is described in this guideline.
Type 2 myocardial infarction is secondary to an imbalance between myocardial oxygen supply and demand. This can arise from conditions such as coronary artery spasm, dissection or embolism as well as tachyarrhythmias, sustained bradyarrhythmias, anaemia, respiratory failure and hypotension, often in the presence of underlying coronary artery disease. There is limited evidence for antiplatelet and anticoagulation therapy in Type 2 myocardial infarction and the risks versus the benefits of treatment must be considered. Management of Type 2 myocardial infarction depends on the underlying cause of oxygen supply–demand mismatch.
Myocardial injury describes an elevated cardiac troponin value that is above the upper limit of normal but does not rise and/or fall and is not associated with evidence of ischaemia or infarction. It is important to recognise that myocardial injury can occur in the absence of myocardial infarction, as a result of many underlying conditions. Myocardial injury can be secondary to cardiac conditions (eg myocarditis, heart failure, Takotsubo cardiomyopathy, cardiac defibrillation) or noncardiac conditions (eg kidney failure, anaemia, sepsis, aortic dissection, pulmonary embolism, stroke, strenuous exercise). Many conditions that cause Type 2 myocardial infarction can also cause myocardial injury in the absence of myocardial infarction. If there is no additional evidence to support the presence of myocardial ischaemia or infarction, a diagnosis of myocardial injury should be made, and underlying causes investigated and managed.
