Periprocedural use of direct-acting oral anticoagulants
Direct-acting oral anticoagulants (DOACs) include factor Xa inhibitors (eg apixaban and rivaroxaban) and direct thrombin inhibitors (eg dabigatran). The large variety of possible surgical procedures and unique patient-related considerations mean that the periprocedural use of DOACs requires clinical judgement, specialist input, and consensus between the treating clinicians. Discuss the risks and expected benefits with the patient.
The need to interrupt DOAC therapy before a procedure depends on the nature of the procedure and patient-related factors (eg kidney function).
If a patient taking a DOAC requires an emergency procedure, rapid reversal of anticoagulant therapy may be required. For information on the reversal of dabigatran, see Bleeding and overanticoagulation with dabigatran. At the time of writing, there is no specific reversal agent accessible in Australia for apixaban or rivaroxaban.
If a patient taking a DOAC is undergoing an elective procedure, assess the procedural bleeding risk to determine whether the procedure has a minimal, low to moderate, or high bleeding riskDouketis, 2022—see Procedure-related factors affecting bleeding risk for more information.
If the procedure has a minimal risk of bleeding (eg minor dental extractions, skin excisions of less than 1 cm, cataract procedures) interruption of DOAC therapy is usually not needed.
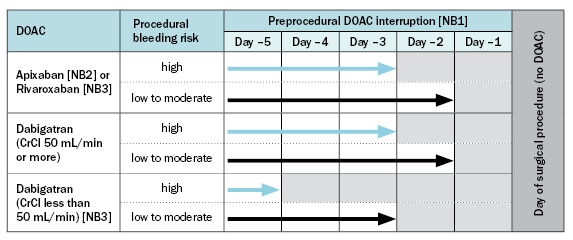
CrCl = calculated creatinine clearance; DOAC = direct-acting oral anticoagulant
NB1: Although these timings are based on patients with atrial fibrillation taking a DOAC at doses recommended for stroke prevention, these recommendations can be applied regardless of the indication. The arrows indicate continuation of DOAC therapy, while the grey cells indicate DOAC therapy is withheld.
NB2: For patients taking apixaban, seek specialist advice if CrCl is less than 25 mL/min—a longer duration of interruption to therapy may be required.
NB3: For patients taking rivaroxaban or dabigatran, seek specialist advice if CrCl is less than 30 mL/min—a longer duration of interruption to therapy may be required. Patients taking rivaroxaban with a CrCl of 15 to 29 mL/min were not included in the relevant studyDouketis, 2019.
If DOAC therapy was interrupted, the timing to restart DOAC therapy after the procedure should be decided in consultation with the proceduralist. Bridging therapy with a parenteral anticoagulant is not recommended for patients restarting a DOAC, because DOACs achieve maximum anticoagulant effect within 1 to 3 hours of the first doseDouketis, 2022Halvorsen, 2022.
For patients who had a procedure with a low to moderate risk of bleeding, DOAC therapy can be restarted 24 hours or more after the procedure if haemostasis has been achievedDouketis, 2019Douketis, 2022.
For patients who had a procedure with a high risk of bleeding, DOAC therapy can be restarted 2 to 3 days after the procedure if haemostasis has been achievedDouketis, 2019Douketis, 2022.
If a prolonged period without DOAC therapy is required (eg no oral intake), consider postoperative VTE prophylaxis or therapeutic parenteral anticoagulationHalvorsen, 2022.
