Assessment of cutaneous drug reactions
Drugs can cause, exacerbate or simulate the full spectrum of skin conditions from pigment disorders to cutaneous lymphoma. Consider a cutaneous drug reaction in any patient with a new onset skin reaction, especially if the patient started a new drug in the preceding days to weeks.
A drug-induced reaction is diagnosed largely on clinical criteria, but laboratory tests can be useful to exclude differential diagnoses. Less severe cutaneous drug reactions with no systemic features usually only need clinical assessment for diagnosis. These reactions do not routinely warrant skin biopsy, and histology is often nonspecific. Skin biopsy can assist with diagnosis of pustular, blistering, vasculitic (eg cutaneous vasculitis), lichenoid, photoallergic and lupus-like reactions.
|
Stevens–Johnson syndrome (SJS) toxic epidermal necrolysis (TEN) | |
|
exanthematic (morbilliform; most common) | |
|
signs and symptoms |
typically begins on trunk and upper limbs polymorphous exanthematic or urticarial lesions on limbs confluent lesions on upper chest purpuric lesions on ankles and feet |
|
typical onset after drug exposure [NB1] [NB2] |
1 week to 1 month |
|
some commonly implicated drugs |
almost all drugs, but most frequent with antibacterials (eg beta lactams, macrolides, quinolones, sulfonamides), many antiepileptics, allopurinol, antiretrovirals, NSAIDs, gold, blood products, cytotoxic drugs |
|
urticarial | |
|
signs and symptoms |
transient erythematous or oedematous patches |
|
typical onset after drug exposure [NB1] [NB2] |
hours to 6 days |
|
some commonly implicated drugs |
antibacterials, NSAIDs (ACEIs trigger angioedema, usually without urticaria) |
|
phototoxic eruption | |
|
signs and symptoms |
presents as an exaggerated sunburn (eg erythema, oedema, blistering, weeping, desquamation) confined to sun-exposed areas |
|
typical onset after drug exposure [NB1] [NB2] |
hours to 2 days |
|
some commonly implicated drugs |
doxycycline, NSAIDs (eg piroxicam, naproxen), amiodarone [NB3], retinoids, sulfonamides, thiazides, griseofulvin, voriconazole |
|
photoallergic eruption | |
|
signs and symptoms |
eczematous or lichenoid can extend beyond sun-exposed areas |
|
typical onset after drug exposure [NB1] [NB2] |
24 to 48 hours after sun exposure |
|
some commonly implicated drugs |
chlorpromazine, piroxicam, thiazides, sulfonylureas, amiodarone, sulfonamides |
|
lichenoid | |
|
signs and symptoms |
widespread, itchy, erythrodermic, scaly, lumpy rash mucous membrane involvement unusual may be photosensitive |
|
typical onset after drug exposure [NB1] [NB2] |
months or even years |
|
some commonly implicated drugs |
ACEIs, beta blockers, chloroquine, ethambutol, gold, hydroxychloroquine, hydroxycarbamide (hydroxyurea), interferon alfa, lithium, methyldopa, penicillamine, sulfonylureas, thiazide diuretics |
|
cutaneous vasculitis | |
|
signs and symptoms |
usually presents as palpable purpura on the lower legs may spread or form plaques, bullae or ulcers |
|
typical onset after drug exposure [NB1] [NB2] |
7 to 21 days |
|
some commonly implicated drugs |
allopurinol, beta lactams, sulfonamides, carbamazepine, diuretics (furosemide [frusemide], thiazides), NSAIDs, phenytoin |
|
fixed drug eruption | |
|
signs and symptoms |
round to oval, sharply marginated, red to violet inflamed plaques that sometimes evolve to blisters solitary or few lesions on face, hands, feet or genital area may involve lips and mouth |
|
typical onset after drug exposure [NB1] [NB2] |
up to 2 weeks (after first exposure) or faster onset (after subsequent exposure) |
|
some commonly implicated drugs |
NSAIDs, sulfonamides, pseudoephedrine, penicillins, tetracyclines, phenobarbital (phenobarbitone), lamotrigine, phenytoin, quinine |
|
Stevens–Johnson syndrome (SJS)—severe cutaneous adverse reaction [NB4] | |
|
signs and symptoms |
significant initial influenza-like symptoms widespread mucocutaneous exfoliation with or without blisters (over 10% of body surface area) |
|
typical onset after drug exposure [NB1] [NB2] |
within weeks (up to 2 months for antiepileptics) |
|
some commonly implicated drugs |
antiepileptics, sulfonamides, allopurinol, NSAIDs, beta lactams |
|
toxic epidermal necrolysis (TEN)—severe cutaneous adverse reaction [NB4] | |
|
signs and symptoms |
significant initial influenza-like symptoms widespread mucocutaneous exfoliation with or without blisters (over 30% of body surface area) |
|
typical onset after drug exposure [NB1] [NB2] |
within 1 week (up to 2 months for antiepileptics) |
|
some commonly implicated drugs |
antiepileptics, sulfonamides, allopurinol, NSAIDs, beta lactams |
|
drug rash with eosinophilia and systemic symptoms (DRESS)—severe cutaneous adverse reaction | |
|
signs and symptoms |
initial influenza-like symptoms exanthematic rash (may also be exfoliative or erythrodermic) nonfollicular pustules facial oedema, lymphadenopathy, peripheral eosinophilia (over 1.5 x 109/L) and internal organ involvement (frequently liver involvement) |
|
typical onset after drug exposure [NB1] [NB2] |
1 to 8 weeks, occasionally up to 4 months |
|
some commonly implicated drugs |
aromatic antiepileptics (phenytoin, carbamazepine, oxcarbazepine), barbiturates, lamotrigine, sulfonamides, dapsone, minocycline, azathioprine, abacavir, nevirapine, allopurinol |
|
acute generalised exanthematous pustulosis (AGEP)—severe cutaneous adverse reaction | |
|
signs and symptoms |
fever, widespread nonfollicular sterile pustules, large areas of oedematous erythema usually starts on the face or axillae marked neutrophilia |
|
typical onset after drug exposure [NB1] [NB2] |
hours to 2 weeks |
|
some commonly implicated drugs |
terbinafine, antibacterials (beta lactams, macrolides, quinolones), calcium channel blockers, antimalarials, pholcodine, paracetamol |
|
Note:
ACEIs = angiotensin converting enzyme inhibitors; NSAIDs = nonsteroidal anti-inflammatory drugs NB1: Typical onset time after drug exposure is based on reported data and expert opinion. NB2: Typical onset time is presented as a range, but most skin reactions occur during the first prolonged exposure to the drug. NB3: Amiodarone can cause slate-blue discoloration of sun-exposed skin. NB4: Stevens–Johnson syndrome and toxic epidermal necrolysis are the same disorders of different severity. | |

Photo sourced with permission from Dr Michelle Goh.

Photo sourced with permission from Dr Michelle Goh.

Photo sourced with permission from Dr Michelle Goh.
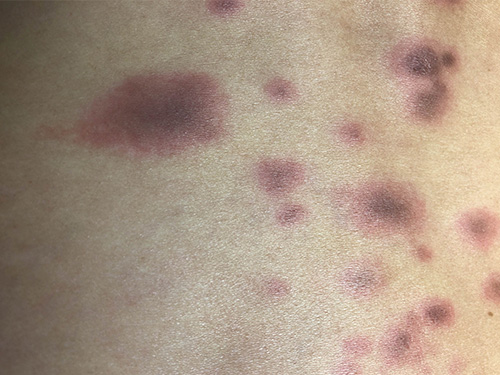
Photo sourced with permission from Dr Andrew Ming.

Photo sourced with permission from Dr Michelle Goh.

Photo sourced with permission from Dr Michelle Goh.

Photo sourced with permission from Dr Michelle Goh.

Photo sourced with permission from Dr Michelle Goh.

Photo sourced with permission from Dr Michelle Goh.
Reactions may be confined to the skin or be part of a systemic reaction (eg fever, sore throat, arthralgia, other systemic symptoms)—systemic features can precede the cutaneous reaction by several days.
Severe cutaneous drug reactions require hospital assessment and treatment. Some signs and symptoms of severe delayed hypersensitivity cutaneous drug reactions includeBalakirski, 2017:
- widespread confluent erythema
- skin pain, blistering, purpura or necrosis
- desquamation of skin when lateral pressure is applied (positive Nikolsky sign)
- rapid progression of skin signs
- mucous membrane involvement (eg eyes [such as conjunctival irritation and photophobia], mouth, genitals [dysuria])
- facial or neck swelling
- headache or neck stiffness
- sore throat
- lymphadenopathy
- fever
- abnormal full blood examination, liver or kidney dysfunction.
Transfer a patient with a suspected severe cutaneous drug reaction to the nearest hospital emergency department for assessment and management; see Management of severe cutaneous drug reactions. See also Drugs commonly implicated in severe cutaneous drug reactions for a list of drugs commonly implicated in severe cutaneous drug reactions.
Otherwise, patients with a suspected less severe cutaneous drug reaction can be managed in primary care; see Management of less severe cutaneous drug reactions.
allopurinol
antiepileptics (eg phenytoin, carbamazepine, oxcarbazepine, phenobarbital [phenobarbitone], lamotrigine)
nonsteroidal anti-inflammatory drugs (NSAIDs)
sulfonamide antibacterials
penicillins
cephalosporins
antiretrovirals (eg abacavir, nevirapine)
proton pump inhibitors (PPIs) [NB1]Casciaro, 2019Lombardo, 2015Salloum, 2021
NB1: Proton pump inhibitors are not as commonly implicated as other listed drugs; however, they are widely prescribed.
