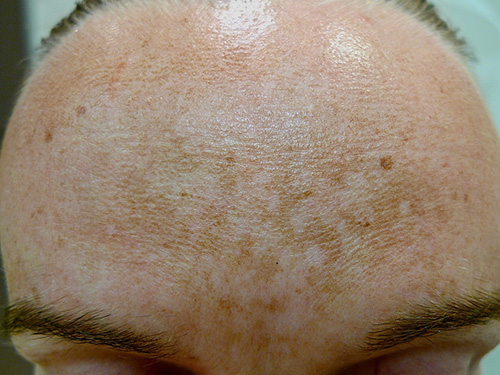
Melasma
Melasma (also known as chloasma) is a common acquired facial hyperpigmentation disorder, typically characterised by irregular brown patches distributed on the upper lip, cheeks and forehead. See here for photos of melasma. It is mainly seen in females with darker skin types; however, it can occur in males and people with any skin type. Melasma is stimulated by sun exposure, and occurs most often during pregnancy or in patients taking hormone therapy (both estrogen and progestogen have been implicated)Lee, 2015Tran, 2020. Hormone therapies include hormonal contraceptives (both oral and non-oral forms) and hormone replacement therapy.




If a hormonal contraceptive is the suspected cause, stopping the contraceptive may be an option. Before stopping therapy, consider how bothersome the melasma is to the patient, how likely the contraceptive is the cause (eg melasma onset coincides with starting a new contraceptive), the patient’s willingness to stop contraceptive therapy, and the likelihood that stopping the contraceptive may not reverse melasma. If the estrogen component of the contraceptive is the suspected cause, alternative options include progestogen-only contraception. Other options may include nonhormonal contraceptives (eg copper intrauterine device [IUD]). Review any changes (eg stopping or switching of contraceptives) after 6 months.
Provide advice on strict sun protection, preferably with physical ultraviolet blockers (eg micronised titanium dioxide, zinc oxide), and tinted sunscreens containing visible light blockers (eg iron oxide)Castanedo-Cazares, 2014.
First-line therapy of melasma is a topical depigmenting agent. Use:
hydroquinone 2% cream topically, once or twice daily for 2 to 4 months1. hydroquinone hydroquinone hydroquinone
Higher concentrations of hydroquinone (eg 4%) can be compounded under dermatologist guidance; however, they should be used for limited periods and under dermatologist supervision because prolonged use of higher concentrations can cause slate-grey skin discolouration.
Do not use topical hydroquinone in patients who are pregnant or breastfeeding because the effects are not well establishedSo, 2020.
If hydroquinone is ineffective, some patients respond to combination therapy with topical tretinoin. To minimise irritation, start by adding a lower strength of tretinoin to hydroquinone, before increasing the strength of tretinoin as tolerated. Add:
tretinoin 0.025% cream topically, at night. Increase to tretinoin 0.05% as tolerated. Review after 4 to 6 months. tretinoin tretinoin tretinoin
Topical retinoids are teratogenic. Avoid topical retinoids in patients who are planning to become pregnant, or who are pregnant. Topical retinoids may be used in patients who are breastfeeding (no data is available, but it is unlikely to be a concern because systemic absorption through the skin is minimal).
Response to therapy is slow, and therapy is often needed for more than 6 months. Relapse after stopping treatment is common, especially with repeated exposure to sun, estrogen or progestogen. If response to combination therapy of hydroquinone and tretinoin is not adequate after 4 to 6 months, refer for dermatologist advice.
Specialist treatments used for melasma include laser treatments, intense pulsed light therapy and chemical peels—expert dermatologist guidance is needed with these treatments.
Although there is emerging evidence for newer generation laser devices in the treatment of melasmaLee, 2018Wong, 2021, the risk of complications (eg postinflammatory hyperpigmentation, rebound or worsening of melasma, confetti-like hypopigmentation and scarring) is significant from all types of physical therapies. Safe use of these therapies requires skilled practitioners (eg dermatologists, practitioners trained by and working under guidance of dermatologists).
Topical and oral tranexamic acid are increasingly being used as specialist treatment of melasma.
