Adjusting insulin dosage
Overview
When adjusting insulin dosage, the basal insulin doses are adjusted first. Once fasting preprandial (before breakfast) glycaemic targets are achieved, bolus insulin doses are adjusted. A multidisciplinary diabetes team should teach the patient to be proactive rather than reactive when adjusting insulin dosage. Changes in insulin dosage may become less frequent as blood glucose concentrations settle; however, day-to-day variations of bolus insulin requirements are normal.
The dose of basal insulin is adjusted by 10 to 20% every 3 to 7 days until fasting capillary (finger-prick) blood glucose concentration targets are achieved.
Doses of bolus insulin are adjusted to achieve postprandial (after a meal) glycaemic targets. Dose adjustments depend on the patient’s:
- intended carbohydrate intake (see Bolus insulin and carbohydrates)
- expected level of physical activity
- blood glucose concentration at that time—incorporating a supplemental (correction) insulin dose if the concentration is above the target range.
The patient must understand that the bolus dose of insulin given before a meal determines the blood glucose concentrations for the 4 to 5 hours after that meal.
Bolus insulin and carbohydrates
For a patient having a fixed carbohydrate intake with meals, the bolus dose of insulin given before the meal can be adjusted by 10 to 20% every 3 to 7 days to achieve either of the following targets:
- 2-hour postprandial (after the meal) blood glucose concentration that the bolus insulin dose was given for
- preprandial blood glucose concentration before the next meal, or at bedtime if related to the dose given for the evening meal. Although less preferable, these preprandial or bedtime measurements are used as an alternative to the 2-hour postprandial blood glucose concentration to minimise the number of daily capillary (finger-prick) blood tests needed (ie four measurements [preprandial and bedtime] rather than seven measurements [preprandial, 2-hour postprandial and bedtime]).
For a patient using carbohydrate counting, the preprandial bolus dose of insulin required to achieve postprandial blood glucose concentration targets is usually calculated based on an insulin-to-carbohydrate ratio (ie the dose of insulin required to cover a set amount of carbohydrate). The ratio varies between individuals, and for an individual at different times during the day. The patient must be taught to calculate the carbohydrate content of their meals by an experienced accredited practising dietitian.
Continuous subcutaneous insulin infusion (CSII) pumps and some blood glucose meters can be preprogrammed with the patient’s insulin-to-carbohydrate ratios. When the patient enters the values for their blood glucose concentration and the amount of carbohydrate they plan to eat, the glucose meter or CSII pump will calculate the required dose of bolus insulin.
If a patient does not have a preprogrammed glucose meter, they can manually calculate their bolus dose of insulin using their insulin-to-carbohydrate ratios (see Example of calculating a bolus insulin dose from an insulin-to-carbohydrate ratio).
A patient with an insulin-to-carbohydrate ratio of 1:10 (1 unit of insulin for every 10 g of carbohydrate) is about to eat 60 g of carbohydrate.
Based on the 1:10 ratio, they will require 6 units (60 ÷ 10) of bolus insulin before the meal.
Supplemental (correction) insulin doses
Supplemental (correction) doses of insulin can be calculated for a patient by taking into account their insulin sensitivity factor. This factor is the calculated drop in blood glucose concentration (in mmol/L) resulting from a supplemental dose of 1 unit of bolus insulin given to that particular patient. For a patient with a stable insulin dosage, the insulin sensitivity factor can be calculated from their total daily insulin dose (sum of all doses of insulin given daily, irrespective of formulation) using the formula:
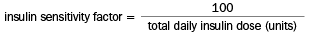
The patient’s insulin sensitivity factor may then need to be revised according to the blood glucose concentration response after a supplemental (correction) bolus dose of insulin is given. For an example of calculating a supplemental dose of insulin using an insulin sensitivity factor, see Example of calculating a supplemental (correction) dose of insulin using an insulin sensitivity factor.
A patient with a total daily insulin dose of 50 units needs to reduce their BGC from 14 to 6 mmol/L—a reduction of 8 mmol/L (14 – 6).
The patient’s insulin sensitivity factor is 2 (100 ÷ 50). One unit of bolus insulin should reduce the patient’s BGC by 2 mmol/L.
To reduce the BGC by 8 mmol/L, give an extra 4 units (8 ÷ 2) of bolus insulin, in addition to the usual dose of bolus insulin required to cover the carbohydrate content of the meal.
BGC = blood glucose concentration
