Approach to managing acute gastroenteritis
Management of acute gastroenteritis is largely supportive and should be individualised based on clinical (and if indicated, laboratory) assessment. It should address the cause of gastroenteritis (if infectious, see Acute infectious diarrhoea) and any clinical features (see Management of clinical features of acute gastroenteritis). Management of acute gastroenteritis in adults and children outlines the approach to managing acute gastroenteritis.
Rehydration is the most important aspect of managing acute gastroenteritis. All patients with gastroenteritis should have their hydration status assessed so that appropriate rehydration can be given (see Assessing adults for dehydration and Assessing children for dehydration). Children, older patients, and those with chronic diseases may rapidly become dehydrated during an episode of gastroenteritis. Dehydration from acute gastroenteritis is a significant cause of death in children in developing countries, and remains a significant reason for hospitalisation in developed countries.
Antibiotics are of no benefit in most cases of acute gastroenteritis and may exacerbate or prolong diarrhoea. For information about the role of antibiotic therapy in acute infectious diarrhoea, see Acute infectious diarrhoea in the Antibiotic guidelines.
Assess all patients (including patients presenting to their general practitioner, hospital inpatients and residents of aged-care facilities) with gastroenteritis symptoms using standard and transmission-based precautions and follow local infection control standards in relation to isolation—see the Australian Guidelines for the Prevention and Control of Infection in Healthcare.
In infectious diarrhoea, notification of public health authorities is important in limiting outbreak size, particularly if the patient lives in a congregate living setting (eg residential aged-care facility), works in the food industry, or attends or works at a childcare facility or school1.
|
Clinical feature |
Management |
|---|---|
|
dehydration |
see Rehydration for acute gastroenteritis in adults and Rehydration for acute gastroenteritis in children |
|
electrolyte imbalance |
assess electrolytes in all patients with:
for information about management of electrolyte imbalance, see Electrolyte abnormalities |
|
vomiting and diarrhoea |
consider symptomatic treatment with antiemetic drugs for acute gastroenteritis and antidiarrhoeal drugs for acute gastroenteritis treatments that may reduce duration of symptoms in children include probiotics and zinc supplements diet and feeding may need to be adjusted during acute illness |
|
perianal excoriation or skin breakdown |
particular risk in patients who develop incontinence, frail patients, and infants or children who are not toilet trained apply a barrier cream or a ‘no-sting’ barrier film to help prevent incontinence-associated dermatitis or excoriationBeeckman, 2016 |
|
medication-related complications | |
|
complications in older or frail patients |
assess risk and develop a management plan to reduce risk of falls, pressure injuries and delirium, and to prevent destabilisation of pre-existing chronic diseases |
|
lactose intolerance following acute illness |
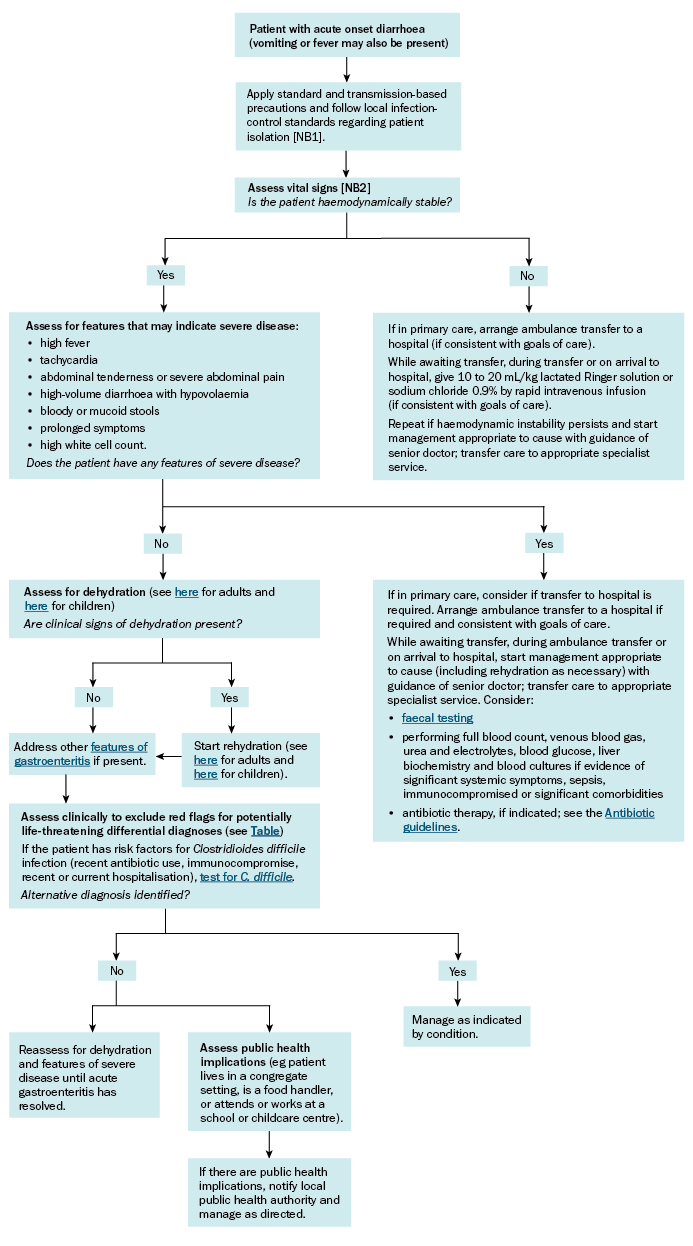
NB1: Assess all patients with gastroenteritis symptoms (including patients presenting to their general practitioner, hospital inpatients and residents of aged-care facilities) using standard and transmission-based precautions and follow local infection control standards in relation to isolation, see the Australian Guidelines for the Prevention and Control of Infection in Healthcare.
NB2: In children, normal ranges for vital signs vary depending on the child’s age; see the Royal Children’s Hospital Melbourne website for acceptable age-based ranges for physiological variables.
