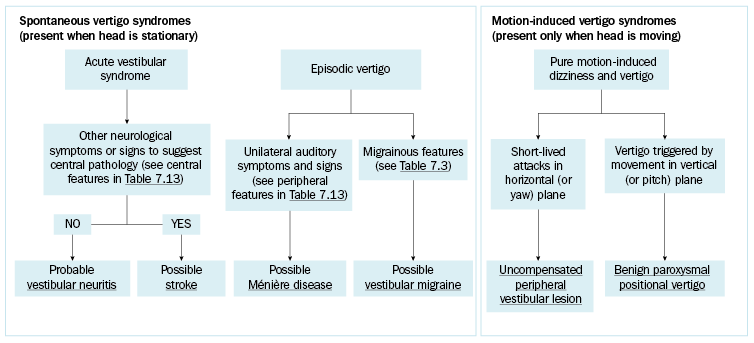
Dizziness and vertigo diagnosis
Dizziness is a broad term used by patients to describe a range of sensations that include vertigo, gait ataxia and presyncope. Vertigo is an illusion of motion and is usually rotatory (ie a spinning sensation), but sometimes linear (ie a sense of falling or pitching). Autonomic symptoms (eg nausea, retching, vomiting, pallor, sweating) often accompany vertigo.
|
Peripheral features |
Central features |
|---|---|
|
hearing loss tinnitus aural fullness positive head impulse test |
gait ataxia out of proportion to extent of vertigo visual field loss diplopia hemisensory loss limb weakness and ataxia slurred speech (dysarthria) difficulty swallowing (dysphagia) eye movement abnormalities (direction-changing nystagmus, skew deviation) |
Note: NB1: For advice on bedside assessment of vertigo (including eye movement abnormalities and the head impulse test), see Welgampola MS, Bradshaw AP, Lechner C, Halmagyi GM. Bedside assessment of acute dizziness and vertigo. Neurol Clin 2015;33(3):551-64, vii. [URL]
| |
[NB1]
Vertigo caused by acute unilateral loss of vestibular function (eg vestibular neuritis) is mostly self-limiting—it improves over hours to days due to central vestibular compensation, even when peripheral vestibular function has not recovered. Some patients still have motion-induced dizziness after the acute vertigo resolves, due to incomplete compensation (see uncompensated peripheral vestibular lesion).
Dizziness can also be due to drugs, postural hypotension and other medical disorders. It can be a somatic symptom in primary psychiatric disorders (eg panic disorder, agoraphobia). Chronic intractable dizziness can occur in persistent postural-perceptual dizziness.
