Treating hyponatraemia
Introduction
Hypovolaemic hyponatraemia (clear-cut sodium and water depletion [eg from diuretic drugs]) may respond to intravenous sodium chloride 0.9%, with potassium supplements if required. Sodium chloride 0.9% has a higher sodium concentration than hyponatraemic plasma. Any drugs implicated as a cause of hypovolaemic hyponatraemia should be stopped before intravenous treatment begins.
Patients with hypervolaemic hyponatraemia who are oedematous due to heart, liver or kidney failure may respond to fluid restriction. A loop diuretic may be added as long as the effective intravascular volume is not depleted further.
Treatment of euvolaemic hyponatraemia is based on:
- the presence of central nervous system symptoms (unconsciousness, seizure, drowsiness, headache)
- the severity
- the rate of development.
Acute severe symptomatic hyponatraemia generally needs treatment with intravenous sodium chloride 3%. Chronic or slowly developing hyponatraemia of the same degree may be managed initially by fluid restriction.
Mild to moderate hyponatraemia
For mild to moderate hyponatraemia in euvolaemic or hypervolaemic patients (serum sodium concentration from 120 to 135 mmol/L, no cerebral symptoms), apply:
fluid restriction (eg restrict to 500 mL to 1 litre per 24 hours, or 500 mL less than daily urine output). Monitor serum electrolytes, creatinine and urine output daily or twice daily.
More aggressive intervention to increase the serum sodium concentration above 120 mmol/L is generally not indicated. Potential causes of hyponatraemia (see Common causes of hyponatraemia) should be identified and treated.
Severe hyponatraemia
For severe hyponatraemia (serum sodium concentration lower than 120 mmol/L or with cerebral symptoms), treatment is intravenous sodium chloride 3% (513 mmol/L). The initial target serum sodium concentration should not be higher than 120 mmol/L.
Rapidly correcting hyponatraemia may produce permanent central nervous system injury, due to osmotic demyelination. Patients with chronic hyponatraemia (ie known duration more than 48 hours) are particularly at risk. Additional factors that increase this risk include:
- serum sodium concentration lower than or equal to 105 mmol/L
- hypokalaemia
- alcoholism
- malnutrition
- advanced liver disease.
To avoid osmotic demyelination, the maximum rate of change in the serum sodium concentration in chronic hyponatraemia should be:
- not more than 10 mmol/L in the first 24 hours
- not more than 18 mmol/L in the first 48 hours.
To reduce the risk of overcorrection, the suggested goal of therapy is even lower: 4 to 8 mmol/L daily. For patients with the additional risk factors listed above, the goal should be 4 to 6 mmol/L daily.
This infusion should be given with critical care monitoring.
More rapid initial correction can be considered in patients with:
- seizures or coma, regardless of whether the hyponatraemia is known to be chronic
- self-induced acute water intoxication (eg psychiatric conditions, endurance exercise)
- known hyponatraemia for less than 24 to 48 hours
- intracranial pathology or increased intracranial pressure.
The goal of therapy in these patients is to raise the serum sodium concentration by 4 to 6 mmol/L, to prevent neurological damage secondary to brain herniation, swelling and cerebral ischaemia. Use:
sodium chloride 3% 100 mL IV over 10 minutes. Repeat as needed up to a maximum of 3 infusions. hyponatraemia (severe) sodium chloride
Often it is difficult to assess whether severe hyponatraemia is acute or chronic. Unless it is clearly acute, a slower rate of correction is advised. The volume of bolus sodium chloride and the patient's response must be considered when calculating the remaining volume and infusion rate in chronic hyponatraemia.
The increase in serum sodium concentration (mmol/L) achieved per litre of infused sodium chloride 3% can be calculated using the formula below1. To calculate total body water, see calculation2.

Sample calculation for rate of infusion of sodium chloride 3% to correct hyponatraemia gives a sample calculation.
patient: 60 kg, 40 years, female
serum sodium concentration: 110 mmol/L
target serum sodium concentration at 24 hours: 118 mmol/L
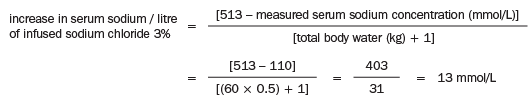
To achieve an increase of 8 mmol/L: infuse 8/13 of 1 litre = 615 mL sodium chloride 3%
To achieve an increase of 8 mmol/L in 24 hours: infusion rate = 615 mL/24 hours = 26 mL/hour
If an initial rapid increase in the serum sodium concentration is needed, for example to achieve 115 mmol/L of serum sodium, the infusion could begin at 64 mL/hour for an anticipated 6 hours and then reduce to 13 mL/hour for the following 18 hours.
If two bolus doses of 100 mL have been given initially, the remaining infusion volume over 24 hours is 615 – 200 mL = 415 mL, so the infusion rate = 17 mL/hour.
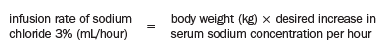
As a quick check of the calculation, the following conservative formula may be used to determine the initial infusion rate (mL/hour) of sodium chloride 3%:
When intravenous sodium chloride 3% is used, the serum sodium concentration should be checked every 4 hours and the infusion rate adjusted as required. Adequate potassium replacement may reduce the risk of demyelination.
When SIADH persists long term (often when it is due to cerebral or pulmonary abnormalities or malignancy), first-line therapy is:
chronic fluid restriction, usually restricting intake to 1 litre daily.
When the patient can't tolerate the degree of fluid restriction needed to maintain a safe serum sodium concentration, drug therapy may be indicated. Two vasopressin receptor antagonists (conivaptan and tolvaptan) have been approved by the United States Food and Drug Administration for treating euvolaemic hyponatraemia. Neither is available in Australia at the time of writing.
