Follow-up and duration of antidepressant therapy for major depression
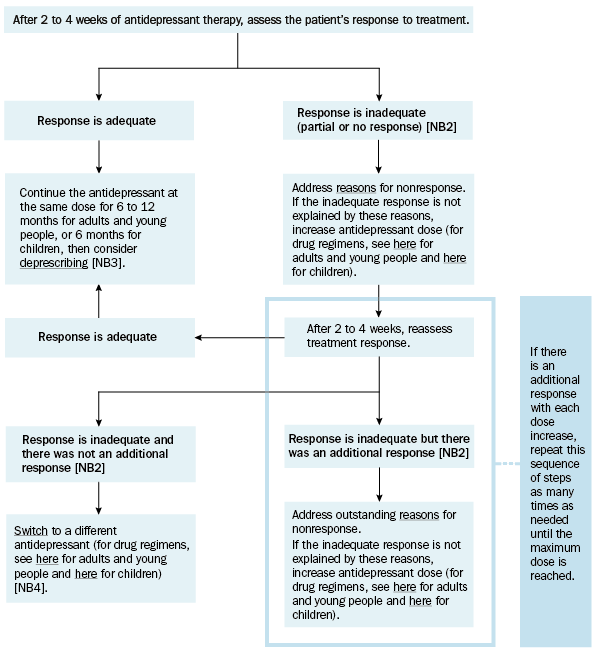
Throughout antidepressant treatment, regularly assess the patient for response to treatment and adverse effects. Monitor patients more frequently at the start of treatment because activation and suicidal thoughts are more common during the first 7 to 10 days.
[NB1]
NB1: If an unacceptable adverse effect occurs at any time, switch to an antidepressant less likely to cause the adverse effect.
NB2: If a low starting dose was used to minimise initial adverse effects (eg nausea, restlessness, agitation), the time to therapeutic effect may be prolonged.
NB3: If a patient has had 2 or more depressive episodes within 5 years, 3 or more cumulative episodes, psychotic depression or a serious suicide attempt, continue antidepressant therapy for 3 to 5 years—sometimes lifelong therapy is required. For adults and young people with recurrent depression (ie more than one episode), also see Recurrent major depression in adults and young people.
NB4: If symptoms persist despite using an effective dose of at least 2 antidepressants as sequential monotherapy, each for a minimum of 4 weeks, see Treatment-resistant major depression in adults and young people or Treatment-resistant major depression in children.
Because there is a high risk of relapse after a single episode of major depression, once an acceptable response is achieved, continue treatment for:
- at least 6 months (preferably 12 months) in adults and young people
- 6 months in children.
It is common for people with major depression to fail to respond to the first antidepressant used. Reinforce to the patient that a trial of more than one antidepressant may be required (given sequentially as monotherapy) before an acceptable response occurs. Inform the patient there is considerable interpatient variability in response to antidepressants. If psychological therapy has not been used, consider a trial, either alone or in combination with an antidepressant.
Consider the following questions if a patient does not respond to an antidepressant [NB1].
- Is the diagnosis correct?
- Have possible medical causes of symptoms been identified and treated?
- Have alcohol or other substance use problems been addressed?
- Have relevant psychosocial factors been addressed?
- Has the patient been treated with an adequate dose of the antidepressant for an adequate duration?
- Is an interacting drug reducing the response? [NB2]
- Is the patient adherent to therapy?
- Have they been taking their antidepressant regularly?
- Is the patient experiencing an adverse effect?
NB1: If a child has not responded to an antidepressant, consider referring them to a paediatrician (or if available, a child psychiatrist or age-appropriate mental health service) for a comprehensive assessment.
NB2: Many antidepressants are metabolised by cytochrome P450 enzymes. Information on drug interactions mediated through these enzymes can be found at the University of Indiana School of Medicine’s drug interaction website.
If depressive symptoms persist despite using an effective dose of at least 2 antidepressants as sequential monotherapy, each for a minimum of 4 weeks, see Treatment-resistant major depression in adults and young people or Treatment-resistant major depression in children.
