Approach to diagnosis of asthma
This topic addresses asthma diagnosis in children 6 years and older as well as adolescents and adults. For assessment of children aged 1 to 5 years with respiratory symptoms suggestive of asthma, see Assessment of wheeze and asthma in children 5 years and younger. Wheezing in infants younger than 12 months is most commonly a symptom of acute viral bronchiolitis rather than asthma. For information about wheeze in infants younger than 12 months, see here.
Asthma is characterised by a variety of respiratory symptoms including wheeze, shortness of breath, cough, chest discomfort or tightness, and, in children, increased respiratory rate and work of breathing. The symptoms vary in intensity and over time. Patients who present with these symptoms should be investigated for asthma. Asthma frequently presents in childhood, but can occur for the first time at any age.
The diagnosis of asthma is based on clinical assessment supported by lung function tests (primarily spirometry) that demonstrate airflow limitation or airway inflammation. Lung function tests have significant false positive and negative results. No single test or symptom can be used to diagnose asthma, and isolated signs or symptoms have poor predictive value. Always record the basis of the diagnosis of asthma.
A diagnosis of asthma should preferably be confirmed before starting regular preventer treatment, as it is harder to confirm the diagnosis once treatment is started. Empirical treatment with an inhaled corticosteroid can be started in patients with significant symptoms or exacerbations, but testing should be done as soon as possible.
If the diagnosis remains uncertain and symptoms persist, refer the patient to a specialist for further investigation.
Assessment of suspected asthma in children 6 years and older, adolescents and adults outlines the steps involved in making a diagnosis of asthma.
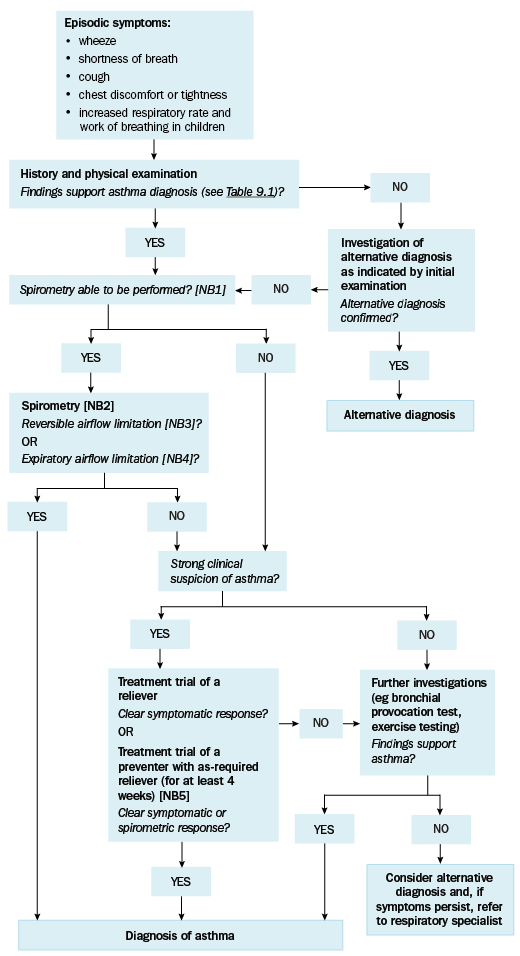
NB1: Spirometry is not always reliable in children, so a treatment trial may be preferred.
NB2: Normal spirometry when the patient is not symptomatic does not exclude the diagnosis of asthma; ideally, repeat spirometry when the patient is symptomatic. If spirometry is normal when the patient is symptomatic, consider an alternative diagnosis. Repeated measurements of lung function are often more informative than a single assessment.
NB3: Reversible airflow limitation is defined as an increase in forced expiratory volume in 1 second (FEV1) of at least 200 mL and at least 12% from baseline 10 to 15 minutes after administration of a short-acting beta2 agonist.
NB4: Expiratory airflow limitation is defined as reduced FEV1 to forced vital capacity (FVC) ratio (FEV1/FVC ratio).
NB5: A preventer can be used in combination with a reliever for a treatment trial.
Adapted from the Australian Asthma Handbook © 2020 National Asthma Council Australia. Accessed 31 August 2020.
