Managing comorbidities
Comorbidities such as obesity, gastro-oesophageal reflux, rhinitis and rhinosinusitis, inducible laryngeal obstruction and anxiety and depression can worsen asthma control or contribute to the risk of exacerbations. Figure 9.3 outlines relevant comorbidities. Managing these conditions can improve asthma control and should always be considered before stepping up asthma therapy.
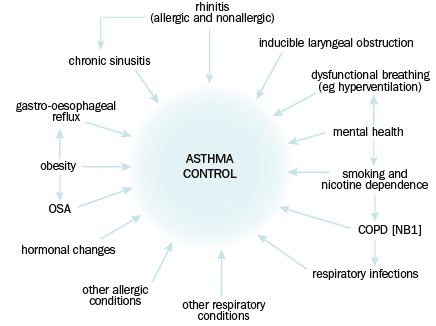
COPD = chronic obstructive pulmonary disease; OSA = obstructive sleep apnoea
NB1: See Overlap of asthma and COPD for further information.
Reproduced with permission of the © ERS 2020. European Respiratory Journal 2009 33:897-906; DOI: 10.1183/09031936.00121308. [URL]
Anxiety disorders and depression
Anxiety disorders and depression are more common in patients with asthma, particularly severe asthma, than in the general population.
Anxiety disorders can be a trigger for asthma symptoms, and can also affect perception of symptoms (eg over perception of symptom severity). Dysfunctional breathing (eg hyperventilation related to a panic attack) can be confused for asthma symptoms. Patients with comorbid asthma and an anxiety disorder may experience worse control of symptoms than other patients with asthma.
Depression can be a risk factor for poor medication adherence and self-management, which can in turn reduce asthma control.
Actively screen for mental health disorders in patients with asthma, particularly severe asthma. For management advice, see Depression and Anxiety and associated disorders.
Obesity
Obesity (defined as a body mass index [BMI] more than 30 kg/m2) is associated with an increased prevalence of asthma. Obese patients are more likely to have obstructive sleep apnoea and gastro-oesophageal reflux, which can also worsen asthma control.
Weight loss of at least 5 to 10% may result in clinically significant improvements in asthma control.
Obese people experience more dyspnoea and asthma-like symptoms than nonobese people—before starting or escalating asthma treatment in an obese patient, confirm that the symptoms are caused by asthma with lung function testing.
Gastro-oesophageal reflux
Patients with asthma have higher rates of gastro-oesophageal reflux. Asthma drugs can cause relaxation of the lower oesophageal sphincter, which can worsen gastro-oesophageal reflux. The presence of gastro-oesophageal reflux can also worsen asthma control or contribute to coughing.
For advice on management of gastro-oesophageal reflux, see here. Treatment of gastro-oesophageal reflux will not necessarily improve asthma symptoms.
Rhinitis and rhinosinusitis
Rhinitis or chronic rhinosinusitus commonly coexists with asthma (sometimes referred to as ‘United Airway Disease’). Asthma occurs in 30% of patients with allergic rhinitis, and allergic rhinitis occurs in more than 80% of patients with allergic asthma.
Assess patients with asthma for rhinitis and rhinosinusitis, particularly if their asthma is related to allergies, or is difficult to control. Poorly controlled rhinitis and rhinosinusitis can worsen asthma control—see Rhinitis and Chronic rhinosinusitis for management advice.
Inducible laryngeal obstruction (upper airway dysfunction or vocal cord dysfunction)
Inducible laryngeal obstruction (also known as upper airway dysfunction or vocal cord dysfunction) results from abnormal and intermittent adduction of the vocal cords or supraglottic muscles during respiration. It can mimic, and is often misdiagnosed as, asthma. The condition presents with intermittent and variable symptoms, including wheeze, dyspnoea and cough. Most patients with inducible laryngeal obstruction experience inspiratory breathing difficulties, and may describe a choking sensation, or a sensation of breathing through a straw. Symptoms can be triggered or worsened by exercise, gastro-oesophageal reflux, chronic rhinosinusitis, irritants (eg pollutants, occupational irritants) and emotional stress.
These episodes can be frightening to the patient. Symptoms do not respond to short-acting beta2 agonists.
Inducible laryngeal obstruction can occur independently or coexist with asthma. If it is not diagnosed and managed, it can worsen asthma control and lead to overtreatment of asthma. If inducible laryngeal obstruction is suspected, seek specialist advice.
