Overview of stepwise therapy for children 6 years and older
Drug therapy for asthma in children 6 years and older is introduced in a stepwise manner, as shown in Stepped approach to starting and adjusting asthma therapy in children 6 years and older. For younger adolescents (younger than 14 years), the recommendations for managing asthma in children described in this topic apply in most situations. For older adolescents, the recommendations for managing asthma in adults apply in most situations; see Maintenance management of asthma in adults and adolescents.
The initial treatment step is determined by the frequency and severity of symptoms. For details about each step, including drug dosages, see the relevant sections—Step 1, Step 2 and Step 3.
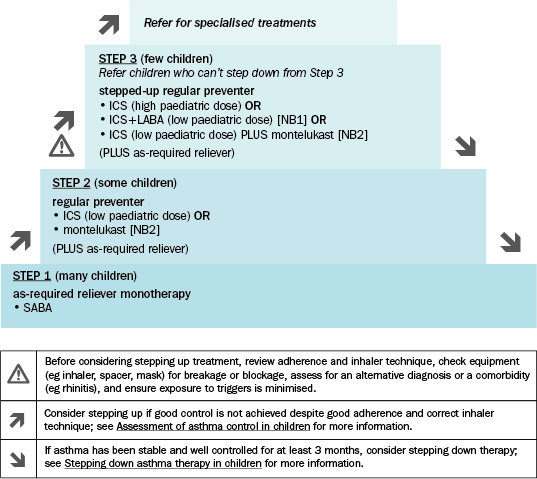
ICS = inhaled corticosteroid; LABA = long-acting beta2 agonist; SABA = short-acting beta2 agonist
NB1: Always give ICS+LABA therapy as a fixed-dose combination inhaler to avoid the possibility of patients taking a LABA without an ICS; LABA monotherapy increases the risk of exacerbations and asthma-related death.
NB2: Montelukast is less effective than ICS and has been associated with neuropsychiatric adverse effects (eg behavioural changes, depression, suicidality). Adverse effects are generally mild and may be coincidental; however, symptoms may be serious and continue if treatment is not stopped. Advise patients, parents and carers to be alert for changes in behaviour and new psychiatric symptoms. Stop treatment if these effects occur. In some cases, symptoms may persist after stopping treatment; patients should be monitored and provided supportive care until symptoms resolve. See the Australian Therapeutic Goods Administration (TGA) safety alert for more information.
Adapted from the Australian Asthma Handbook © 2020 National Asthma Council Australia. Accessed 31 August 2020.
Review symptom control 4 to 6 weeks after starting therapy to determine whether good control has been achieved. A continuous cycle of reviewing response and adjusting therapy (stepping up or down) is recommended, aiming to achieve a normal quality of life using the minimal dose regimen. See Review and ongoing management of asthma in children.
