Summary of management of acute asthma
The management of acute asthma in a clinical setting is summarised in Summary of management of acute asthma.
Management is determined by the severity of the exacerbation. At presentation, immediately perform a rapid severity assessment of the patient to determine initial management. After starting treatment, perform a more detailed secondary severity assessment to determine ongoing management. Continuously reassess severity and response to therapy. If the patient is not responding to treatment at the assessed severity level, escalate treatment to the next level.
Bronchodilator therapy (eg salbutamol, ipratropium) is the mainstay of treatment of acute asthma. Oral corticosteroid therapy is also recommended for most patients—see Corticosteroid therapy for acute asthma for details.
Oxygen is used if the patient is hypoxaemic, and intravenous magnesium sulfate can be considered if the patient does not respond to initial treatment.
For detailed information on the management of acute asthma by severity, including drug dosages, see:
- Treatment of mild to moderate acute asthma
- Treatment of severe acute asthma
- Treatment of life-threatening acute asthma.
Antibiotic therapy has no role in the management of acute asthma unless the patient has strong evidence of lung infection (eg radiographic evidence of pneumonia). Oral beta2 agonist therapy also has no role.
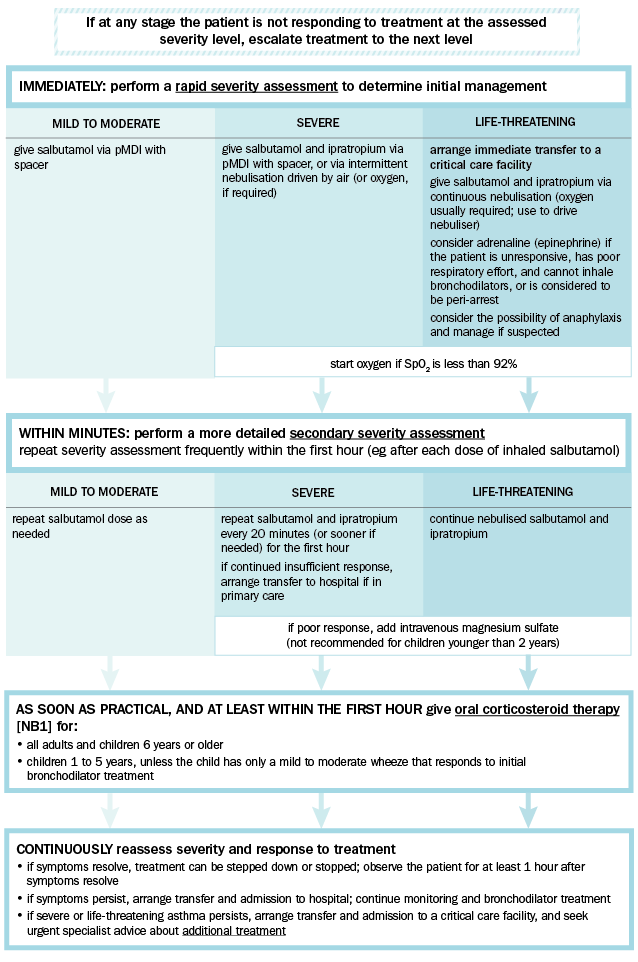
pMDI = pressurised metered dose inhaler; SpO2= oxygen saturation measured by pulse oximetry
NB1: Use intravenous corticosteroid therapy if oral intake is not tolerated.
Adapted from the Australian Asthma Handbook © 2020 National Asthma Council Australia. Accessed 31 August 2020.
Mild to moderate exacerbations can usually be managed in the primary care setting. Consider escalating the level of care according to the severity, response to initial treatment, limitations of the current care setting, and ease of access to more advanced assistance. In the emergency department, early involvement of senior staff is desirable for very sick patients. If transfer to a higher-level facility is anticipated, start this process early.
Review the diagnosis if the patient does not respond to therapy. If the patient appears to respond initially and then relapses, consider the possibility of complications such as pneumothorax. Also consider adverse effects of treatment—high doses of salbutamol can cause paradoxical worsening of respiratory failure (thought to be related to metabolic acidosis, increased blood lactate concentration and increased metabolic rate). If suspected, seek expert advice and cautiously reduce salbutamol dosage.
Hypokalaemia and hypomagnesaemia are likely with repeated high doses of salbutamol—anticipate and manage early. Cardiovascular effects (eg myocardial ischaemia, prolonged QT interval predisposing to arrhythmias) can also occur.
