Approach to management of allergic rhinitis
In patients with allergic rhinitis caused by a clinically obvious allergen, minimise exposure to the allergen if possible. Exclude other causes of rhinitis, such as rhinitis medicamentosa caused by overuse of intranasal decongestants.
Approach to management of allergic rhinitis outlines the approach to management of allergic rhinitis.
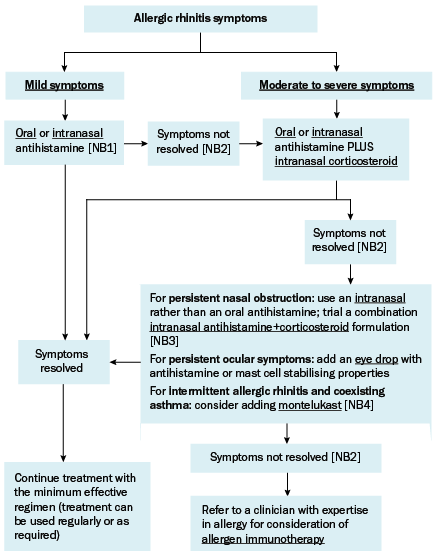
NB1: Combining oral and intranasal antihistamine therapy does not confer additional benefit compared with using either one alone.
NB2: Trial new treatments for around 4 weeks before assessing response. Before escalating treatment, assess adherence and, if using a nasal spray, assess technique (see Patient instructions for using a nasal spray for patient instructions for using a nasal spray). Also consider alternative diagnoses, particularly if the patient has no response to standard therapy.
NB3: Oral and intranasal decongestants have no role in allergic rhinitis and should be avoided.
NB4: Triple therapy with an antihistamine, an intranasal corticosteroid and montelukast can be trialled before referral, but this is usually less effective than allergen immunotherapy.
Once symptoms have resolved, continue treatment with the minimum effective regimen; treatment can be used regularly or as required. Tailor the duration of treatment to the patient’s symptoms. Patients with intermittent symptoms that occur seasonally may only require treatment for a few months of the year, while others may require long-term treatment.
For patients who do not have an adequate response to treatment, check the patient’s adherence and nasal spray technique (see Patient instructions for using a nasal spray). Also consider the possibility of an alternative diagnosis, particularly in patients who have no response to treatment. Features that suggest an alternative diagnosis include unilateral symptoms, nasal obstruction without other symptoms, pain, purulent discharge, recurrent epistaxis and loss of sense of smell.
If the patient does not have any features that indicate an alternative diagnosis, refer them to a clinician with expertise in allergy for consideration of allergen immunotherapy.
Computed tomography (CT) scans are not recommended for uncomplicated rhinitis as they are costly and expose the patient to radiation. If an alternative diagnosis is suspected, or if the patient has complications of rhinitis, consider a CT scan of the sinuses and referral to an ear, nose and throat surgeon for consideration of surgery.
For videos demonstrating correct use of nasal sprays, see the National Asthma Council website.
To use a nasal spray effectively and safely, follow these instructions:
- If the spray device is new or has not been used for more than a few days, prime the device according to the manufacturer’s instructions.
- Shake the bottle.
- Clear the nasal passages first by gently blowing your nose (or by using a saline rinse to clear nasal obstruction and then waiting for 10 minutes before using the nasal spray).
- Bend your neck forward and look down.
- Put the nozzle just inside the nose, aiming towards the outer wall of the nose and the ear (away from the middle or the top of the nose). Use your right hand for the left nostril and left hand for the right nostril. This reduces the amount of drug deposited onto the wall that separates your nostrils (septum).
- Press to spray and sniff gently at the same time—sniffing hard can make the liquid go straight down the throat.
If you are using two different nasal sprays, wait 10 minutes between sprays.
