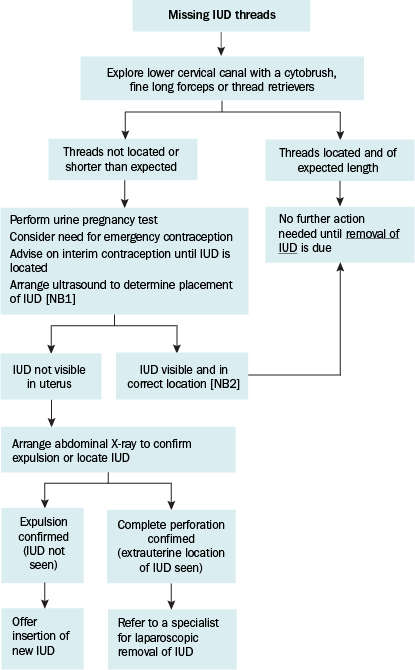
Managing missing, shortened or lengthened IUD threads
Missing IUD threads may indicate uterine perforation or an expelled or malpositioned IUD. Shortened threads may indicate uterine perforation, or a malpositioned IUD. Lengthened threads may indicate a nonfundally positioned (low-lying) IUD. Advise users to regularly check for the presence of the threads and to seek medical attention if the threads cannot be felt or thread length has changed.
For advice on investigating missing IUD threads, see Managing missing intrauterine contraceptive device threads. Advise use of a barrier method of contraception until the presence and position of the IUD can be confirmed.
Before investigating missing IUD threads, confirm that the IUD inserted has threads (some IUDs available overseas do not have threads).
IUD = intrauterine contraceptive device
NB1: Consider the possibility of an early undetectable pregnancy. If pregnancy is excluded or the patient would proceed to abortion, request the radiologist to proceed to X-ray if the IUD is not visible in the uterus.
NB2: If the IUD is visible but partially perforated (embedded) or significantly malpositioned, see text following Figure 20.2.
Uterine perforation by an IUD can be either partial (embedded in the myometrium [can include some perforation into the pelvic or abdominal cavity]) or complete (free floating in the pelvic or abdominal cavity). Uterine perforation occurs in 0.2% of IUD insertions. Perforation risk is increased during breastfeeding (up to six-fold), and in the first 9 months after delivery regardless of breastfeeding.
If complete perforation is confirmed, refer for laparoscopic removal.
If a partially perforated (embedded) IUD is identified on ultrasound, it should generally be removed; this can often be done easily with gentle traction but may require referral for removal under ultrasound guidance. A discussion with the radiologist or a specialist may assist with the decision. The myometrium is likely to heal quickly; seek specialist advice about when to replace the IUD.
Nonfundally malpositioned (low-lying) IUDs can present with a change in length of the threads, or unusual pain or bleeding. If any of the stem of the IUD is visible in the cervical canal, the IUD must be removed and replaced. Otherwise, organise an ultrasound to assess the position of the IUD, advise on the need for additional contraception and consider the need for emergency contraception until location is confirmed. If an IUD is 20 mm or more below the fundus, contraceptive effect may be reduced; this is particularly the case for the copper IUD. The decision to remove and replace a low-lying IUD is made on a case-by-case basis and depends on background fertility and willingness to use an additional barrier method of contraception.
Around 5% of IUDs are expelled. If reinsertion after expulsion is desired, organise a pelvic ultrasound to check for distortion of the uterine cavity that could increase the risk of expulsion. Advise that there is a higher risk of expulsion of a second IUD.
