Assessment of arterial leg ulcers
For a structured approach to assessing patients with a leg ulcer, see Assessing patients with an ulcer or wound and Overview of assessment and management of arterial leg ulcers.
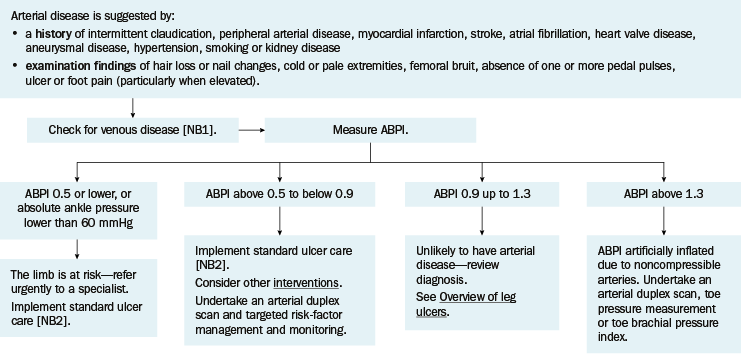
ABPI = ankle brachial pressure index
NB1: Refer patients for a comprehensive venous duplex scan because most leg ulcers are caused by venous disease.
NB2: Standard ulcer care is wound debridement and cleansing, diagnosing and minimising oedema, treating infection (if present), and optimising moisture balance.
A patient with an arterial leg ulcer may have the following clinical features:
- history of vascular disease (cardiac, cerebral, peripheral)
- signs of ischaemia (cold, pale extremities; thin hairless skin)
- pallor on elevation, redness on dependency
- abnormal ankle brachial pressure index (ABPI) (usually less than 0.9, but ABPI may be artificially inflated because arteries are calcified and noncompressible—most commonly from diabetes or kidney disease).
Leg ulcers due to peripheral arterial disease are often painful—pain is aggravated by elevation and relieved by lowering the leg (eg over the side of the bed).
An arterial leg ulcer is shown in Example of an arterial leg ulcer. An arterial leg ulcer may have the following features:
- location—usually toes, bony prominences, sides of feet, heel
- edge—punched out
- base—sloughy or covered by eschar
- exudate—minimal.
In severe cases, an arterial ulcer may be associated with gangrene.

Assess patients with peripheral arterial disease for signs of haemodynamic compromise. Palpation of peripheral arterial pedal pulses (dorsalis pedis and posterior tibial) and auscultation for a femoral artery bruit has a high positive predictive value (93.8%) for the detection of peripheral arterial disease. If femoral bruit is absent and peripheral pedal pulses are present in both lower limbs, the patient is unlikely to have peripheral arterial disease.
Measuring the ABPI accurately detects peripheral arterial disease in most patients and provides prognostic information (see Vascular assessment and ABPI). An ABPI less than 0.9 indicates peripheral arterial disease.
Patients with an arterial leg ulcer and an ankle pressure less than 60 mmHg or an ABPI 0.5 or less have a threatened limb (see Critical limb ischaemia) and need urgent assessment by a vascular specialist. Patients with diabetes require early specialist referral as they may have critical limb ischaemia at higher ankle pressures due to the presence of neuropathy and infection.
For patients with an ABPI less than 0.9, undertake an arterial duplex scan to assess the anatomy of disease.
An ABPI higher than 1.3 does not exclude arterial disease because arteries can be calcified and noncompressible, most commonly due to diabetes, age over 75 years and kidney disease. For patients with an ABPI greater than 1.3, a toe pressure or toe brachial pressure index (TBPI) can be used to assess for arterial disease and likelihood of wound healing—see Interpretation of lower-limb pressure measurements for interpretation.
Refer patients with a leg ulcer for a comprehensive venous duplex scan to detect venous insufficiency because most leg ulcers are caused by venous disease, and chronic venous insufficiency can delay healing.
