Principles of managing CAP in adults
Management of adults with community-acquired pneumonia (CAP) provides an overview of the management of community-acquired pneumonia (CAP) in adults.
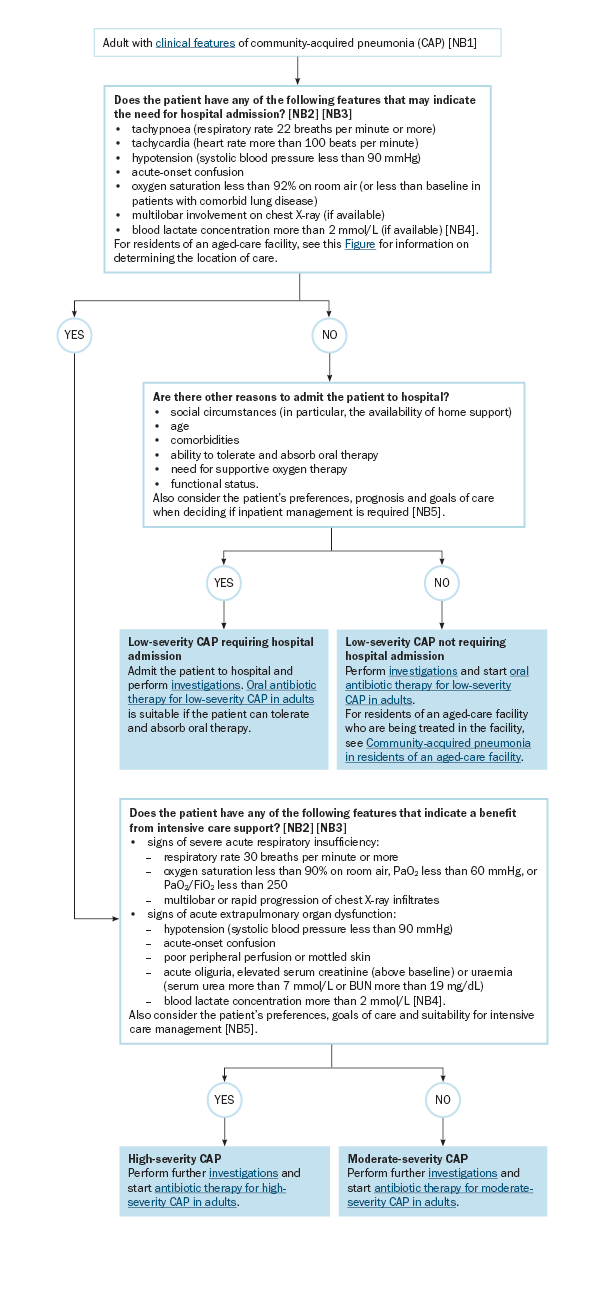
BUN = blood urea nitrogen; FiO2 = fraction of inspired oxygen; PaO2 = partial pressure of oxygen
NB1: CAP is pneumonia that develops in patients in the community, or in patients who have been in hospital for less than 48 hours. In this topic, CAP includes suspected aspiration pneumonia, residents of an aged-are facility who develop pneumonia in the facility but are treated in hospital, and ambulant patients who develop pneumonia in a subacute-care setting (eg rehabilitation). Treat as for hospital-acquired pneumonia if pneumonia develops in a patient who has been either hospitalised in acute care for longer than 48 hours, or discharged within the previous 7 days from a hospital admission of longer than 48 hours.
NB2: Assessment of pneumonia severity and comorbidities is essential to guide empirical antibiotic therapy and the location of care – see Severity assessment of CAP in adults.
NB3: Many of these features are derived from formal pneumonia severity scoring tools. Based on the opinion of the Antibiotic Expert Group, some parameters are more conservative than the scoring tools to enable early identification of patients at risk of deterioration. Also consider if the patient has had a significant change from baseline.
NB4: Blood lactate can be measured using arterial or venous blood gas analysis. Venous blood gas analysis is acceptable for rapid lactate assessment (for further advice, see the Respiratory guidelines).
NB5: Reviewing the patient’s advance care plan, if in place, can assist with treatment decisions, including location of care. See Advance care planning and Pneumonia in palliative care.
