General approach to managing hospital-acquired sepsis or septic shock of unknown source in children 2 months or older
The choice of antibiotics for hospital-acquired sepsis or septic shock in children 2 months or older is complex. A regimen based on local protocols, or advice from a clinical microbiologist or infectious diseases physician improves outcomes. This is particularly important for children in the intensive care unit. Mortality is decreased when appropriate antibiotics are given early.
For advice on recognising sepsis and septic shock, see Identifying sepsis or septic shock, and for advice on early management, see Resuscitation of patients with sepsis and septic shock.
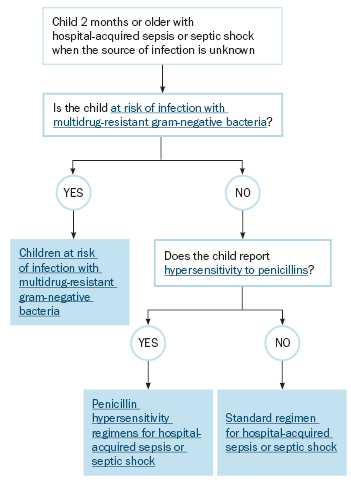
To find the right empirical antibiotic regimen for children 2 months or older with hospital-acquired sepsis or septic shock of unknown source, use Finding the right empirical antibiotic regimen for children 2 months or older with hospital-acquired sepsis or septic shock of unknown source.
The empirical antibiotic regimens in these guidelines can be used initially if local protocols are not available, or if clinical microbiology or infectious diseases advice is not immediately available. The empirical regimens may need to be modified according to local epidemiology, if known. Consideration should also be given to the child’s recent culture and susceptibility test results, whether the child has neutropenia or immune compromise, and whether toxic shock syndrome is suspected. Also consider the addition of an antifungal for children at risk of invasive Candida infection.
Modify therapy as soon as additional information is available (eg source of infection, results of Gram stain, culture and susceptibility testing). Evaluate the appropriateness of antimicrobial therapy daily, with consideration given to the patient’s clinical status and the principles of antimicrobial stewardshipBurston, 2017.