Management of patients reporting hypersensitivity to penicillins
Management of patients reporting hypersensitivity to penicillins depends on many factors. Consider whether antimicrobial therapy is necessary, and the balance of benefits and harms.
Approach to assessment and management of patients reporting hypersensitivity to penicillins in whom a beta-lactam antibiotic is the preferred drug provides a guide for clinicians to classify penicillin hypersensitivity reactions; subsequent antibiotic choice is described for patients with:
- immediate severe penicillin hypersensitivity
- immediate nonsevere penicillin hypersensitivity
- delayed severe penicillin hypersensitivity
- delayed nonsevere penicillin hypersensitivity.
The guidance in this topic is a simplified summary of a complex clinical problem; the Antibiotic Expert Group recognises that there are variations in how penicillin hypersensitivity is managed, and that specialists may choose to manage patients differently after weighing up the benefits and harms in an individual.
When selecting an antimicrobial in a patient with penicillin hypersensitivity, it is important to understand how R1 side-chains affect the risk of cross-reactivity between beta lactams – see Cross-reactivity between penicillins and cephalosporins.
Time since the hypersensitivity reaction is an important consideration when managing patients reporting penicillin hypersensitivity because allergic response wanes over time. Allergy assessment tools (eg PEN-FAST Penicillin allergy decision rule for adults, Beta-lactam antibiotic allergy assessment tool) use the time since the hypersensitivity reaction as a way of stratifying the risk of allergyStevenson 2020Trubiano 2020.
For management of patients with a history of cephalosporin hypersensitivity, seek expert advice.
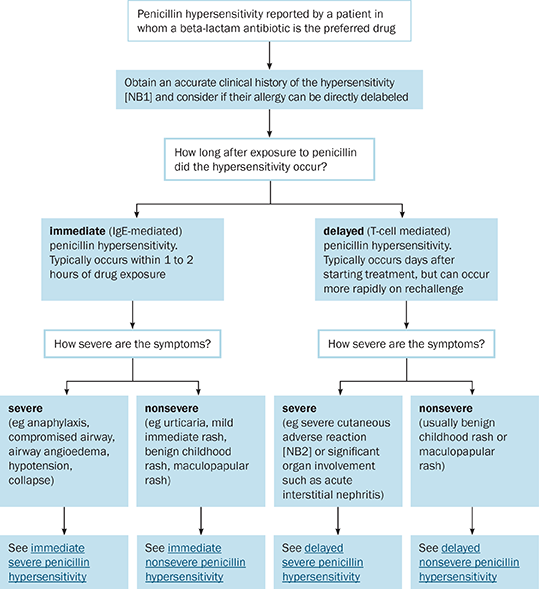
NB1: PEN-FAST Penicillin Allergy Decision Rule and the Beta-lactam antibiotic allergy assessment tool can be used to assess the patient’s penicillin allergy risk.
NB2: Examples of severe cutaneous adverse reactions include drug rash with eosinophilia and systemic symptoms [DRESS], Stevens–Johnson syndrome / toxic epidermal necrolysis [SJS/TEN], severe blistering or desquamative rash.
Avoid:
- penicillins (eg amoxicillin, ampicillin, benzylpenicillin, dicloxacillin, flucloxacillin, phenoxymethylpenicillin, piperacillin)
- in community-based patients, cephalosporins (eg cefalexin, cefalotin, cefazolin, cefepime, cefotaxime, cefoxitin, ceftazidime, ceftriaxone, cefuroxime)
- cefalexin in patients with immediate severe penicillin hypersensitivity to amoxicillin or ampicillin
Safe to administer:
- for directed therapy in hospitalised patients, a cephalosporin (eg cefalexin [NB3], cefalotin, cefazolin, cefepime, cefotaxime, cefoxitin, ceftazidime, ceftriaxone, cefuroxime) should be used if evidence shows treatment with a beta-lactam antibiotic is superior to a non–beta-lactam antibiotic
- non–beta-lactam antibiotics
- aztreonam
Consider:
- for empirical therapy in hospitalised patients, a cephalosporin (eg cefalexin [NB3], cefuroxime, cefazolin, cefalotin, cefoxitin, ceftriaxone, cefotaxime, ceftazidime, cefepime) may be used if evidence shows treatment with a beta-lactam antibiotic is superior to a non–beta-lactam antibiotic
- carbapenems (eg imipenem, meropenem, ertapenem)
- penicillin desensitisation if therapy with a penicillin is essential
NB1: The definitions of immediate hypersensitivity and severe hypersensitivity are listed in Common terminology used when discussing antimicrobial hypersensitivity.
NB2: In a non-urgent situation, consider allergy testing and oral challenge under specialist supervision (where such testing is available).
NB3: Cefalexin is not safe to administer to patients with amoxicillin or ampicillin hypersensitivity.
Avoid:
- penicillins (eg amoxicillin, ampicillin, benzylpenicillin, dicloxacillin, flucloxacillin, phenoxymethylpenicillin, piperacillin)
Safe to administer:
- cephalosporins (eg cefalexin [NB3], cefalotin, cefazolin, cefepime, cefotaxime, cefoxitin, ceftazidime, ceftriaxone, cefuroxime)
- aztreonam
- carbapenems (eg ertapenem, imipenem, meropenem)
Consider:
- penicillin desensitisation if therapy with a penicillin is essential
NB1: The definitions of immediate hypersensitivity and nonsevere hypersensitivity are listed in Common terminology used when discussing antimicrobial hypersensitivity.
NB2: Obtain an accurate hypersensitivity history. PEN-FAST Penicillin Allergy Decision Rule and the Beta-lactam antibiotic allergy assessment tool can be used to assess the patient’s penicillin allergy risk. Consider if the patient’s allergy can be directly delabeled. Consider allergy testing and oral challenge under specialist supervision (where such testing is available).
NB3: Cefalexin may be used in patients who have had a nonsevere (immediate or delayed) reaction to amoxicillin or ampicillin. However, because cross-reactivity between these drugs is possible, consideration should be given to the extent of the reaction, patient acceptability, and the suitability of non–beta-lactam options.
Avoid:
- penicillin (eg amoxicillin, ampicillin, benzylpenicillin, dicloxacillin, flucloxacillin, phenoxymethylpenicillin, piperacillin)
- cephalosporin (eg cefalexin, cefalotin, cefazolin, cefepime, cefotaxime, cefoxitin, ceftazidime, ceftriaxone, cefuroxime)
- penicillin desensitisation
Safe to administer:
- non–beta-lactam antibiotics
- aztreonam
Consider:
- carbapenem (eg ertapenem, imipenem, meropenem)
NB1: The definitions of delayed hypersensitivity and severe hypersensitivity are listed in Common terminology used when discussing antimicrobial hypersensitivity.
Avoid:
- penicillins (eg amoxicillin, ampicillin, benzylpenicillin, dicloxacillin, flucloxacillin, phenoxymethylpenicillin, piperacillin)
Safe to administer:
- cephalosporins (eg cefalexin [NB3], cefalotin, cefazolin, cefepime, cefotaxime, cefoxitin, ceftazidime, ceftriaxone, cefuroxime)
- aztreonam
- carbapenems (eg ertapenem, imipenem, meropenem)
NB1: The definitions of delayed hypersensitivity and nonsevere hypersensitivity are listed in Common terminology used when discussing antimicrobial hypersensitivity.
NB2: Obtain an accurate hypersensitivity history. PEN-FAST Penicillin Allergy Decision Rule and the Beta-lactam antibiotic allergy assessment tool can be used to assess the patient’s penicillin allergy risk. Consider if the patient’s allergy can be directly delabeled. Consider allergy testing and oral challenge under specialist supervision (where such testing is available).
NB3: Cefalexin may be used in patients who have had a nonsevere (immediate or delayed) reaction to amoxicillin or ampicillin. However, because cross-reactivity between these drugs is possible, consideration should be given to the extent of the reaction, patient acceptability, and the suitability of non–beta-lactam options.
