Advice for managing psoriasis in primary care
When a patient presents with psoriasis in primary care, in addition to drug treatment, consider:
- the psychological impact—this is commonly unrecognised and not acknowledged. Psychological impact is often marked, and does not always correlate with severity
- a medication review—certain drugs can trigger or exacerbate psoriasis
- any psoriatic comorbidities (eg cardiovascular disease risk factors, psoriatic arthritis, inflammatory bowel disease, ocular disease). Consider cardiovascular disease risk management and providing lifestyle advice (eg stress management, exercise, weight loss, smoking cessation, reduced alcohol intake, diabetes screening)Mosca, 2015
- undiagnosed infections, including HIV. Severe and recalcitrant psoriasis are indicator conditions for HIV testing1. If severe or recalcitrant psoriasis is identified, offer HIV testing, regardless of whether the patient has behavioural or epidemiological risk factors for HIV infection.
Consider the need for early referral to a dermatologist for advice and consideration of specialist treatments, such as biological therapy. Consider early referral if:
- the patient is very unwell
- psoriasis covers a significant body surface area
- lesions show pustulation (less defined red plaques with scale and pus)
- psoriasis is persistent and not responsive to treatment.
Psoriasis cycles between acute flares and remissions. Drug treatment needs to be variable and appropriate to severity and distribution of disease. Some patients choose not to have drug treatment for mild psoriasis when the symptoms are not troublesome. A patient’s preference for treatment often changes at different times in their life.
If treatment is used for plaque psoriasis, treat according to the location of psoriasis. For treatment of other types of psoriasis (eg guttate psoriasis, generalised pustular psoriasis, erythrodermic psoriasis), see here.
[NB1]
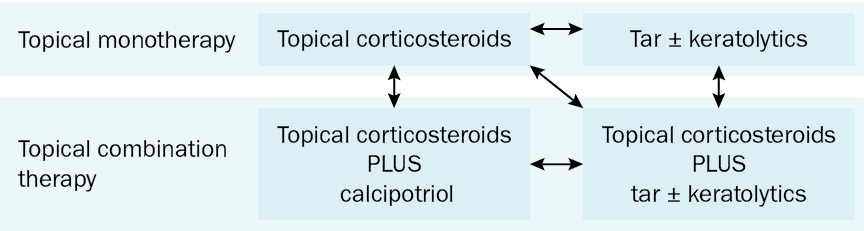
NB1: Rotation and combination of treatment options (as opposed to continuous therapy with one treatment option) is often required when treating psoriasis to minimise adverse effects and to maximise efficacy.
Patients with psoriasis are often prescribed inadequate quantities of topical preparations. Ensure the quantity of preparation prescribed is sufficient to allow coverage of the affected area for the required duration. For example, as a guide for larger areas of application, a single application of topical corticosteroids to the whole body of an average adult requires approximately 30 g of cream or 20 g of ointment. For smaller areas of application, fingertip units can be used as a guide depending on area of application. For more information on application quantities and fingertip units, see here.
Cautious sun exposure is beneficial.
Special diets do not have a role in psoriasis therapy. However, a gluten-free diet may improve the severity of psoriasis in patients with coeliac disease or gluten sensitivity, but it is not a cure.
Information on psoriasis is available to patients on the Psoriasis Australia website.
If therapy available in primary care is not effective, refer to a dermatologist for consideration of specialist treatments, such as biological therapy—see Psoriasis therapy used by dermatologists. Although methotrexate can be prescribed in primary care for severe psoriasis, therapy should be initiated by, or prescribed in conjunction with, a dermatologist.
