Pharmacological interventions
Considerations before prescribing
For advice on assessing and managing an acute behavioural disturbance, see here.
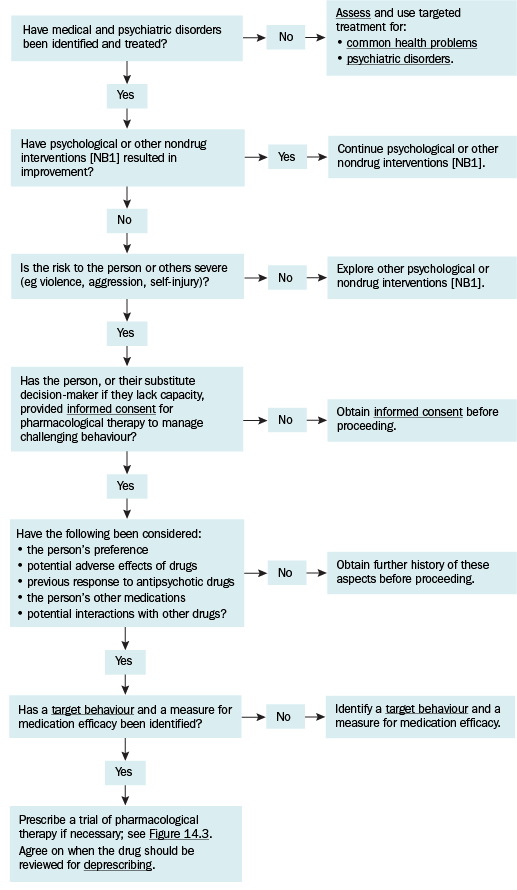
Pharmacological therapy for challenging behaviour in a person with developmental disability should only be considered when the risk to the person or others is severe (eg violence, aggression, self-injury) and when no specific cause or contributor to the challenging behaviour can be identified or managed (eg physical, psychological, neurodevelopmental disorder, communication need, environmental factor); see Commonly missed causes of challenging behaviour in people with developmental disability for commonly missed causes of challenging behaviour in people with developmental disability. Pharmacological therapy for challenging behaviour may be appropriate in children or adults when symptoms are severe, or while waiting for psychosocial or behavioural interventions to be developed or to take effect. It might also be used as an adjunct to a psychosocial or behavioural intervention, to enable the person to best respond to the intervention.
Before prescribing pharmacological therapy to manage challenging behaviour for a person with developmental disability, obtain informed consent. Discuss the indications and adverse effects of drugs with the patient, their family and carers, and their support or substitute decision maker as relevant. Pharmacological therapy for challenging behaviour is considered to be chemical restraint—for legal requirements related to prescribing, see Restrictive practices, the law, and the responsibility of the doctor.
Preparing to prescribe pharmacological therapy for challenging behaviour in a person with developmental disability outlines preparation before prescribing that should be followed after the initial assessment has been completed; see Considerations when assessing and managing challenging behaviour in a person with developmental disability for considerations when assessing and managing challenging behaviour. A systematic approach to prescribing is recommended because the causes of challenging behaviour may be difficult to ascertain, and are often missed in people with developmental disability. Identify the target behaviour and a measure for efficacy of the pharmacological intervention.
The choice of an antipsychotic drug for challenging behaviour requires careful consideration and must take into account factors including the type of behaviour being targeted, drug formulation, cost, adverse effect profile and individual patient factors. People with developmental disability often have obesity, constipation, poor oral and dental health, and mobility problems, and antipsychotic drugs can compound these problems; see Management of antipsychotic adverse effects. Even at low doses, the sedative effects of antipsychotic drugs can mask symptoms of psychiatric disorders, prompt new challenging behaviour and impair the person’s ability to engage with a behaviour support plan (eg their capacity to engage in new learning), affecting longer-term prospects for behaviour change.
In children, pharmacological therapy for challenging behaviour should be started and managed by a clinician with expertise in using psychotropic drugs in children (eg child psychiatrist, paediatrician, other physician, general practitioner). Risperidone is approved by the Australian Therapeutic Goods Authority (TGA) for adults and children over 5 years of age for challenging behaviour1.
Risperidone or aripiprazole2 are approved by the TGA for use in children and adolescents with autism spectrum disorder with challenging behaviour, see Challenging behaviour in a child or adolescent with autism spectrum disorder. For general management advice for people with autism spectrum disorder, see Autism spectrum disorder.
Prescribing a trial of pharmacological therapy for challenging behaviour in a person with developmental disability outlines the process for starting and monitoring a trial antipsychotic drug for challenging behaviour.
If an antipsychotic drug is considered appropriate for challenging behaviour in children or adults with developmental disability, start a time-limited trial with periodic review for efficacy and adverse effects after 3 weeks and 6 weeks. Adjust the dose slowly according to response. If there is evidence of efficacy and the drug is tolerated, continue the antipsychotic drug. If there is no response, stop the antipsychotic drug and seek expert advice. If there is partial response, seek expert advice. See also Monitoring and reviewing strategies.
Chlorpromazine is approved for use in Australia for children with challenging behaviour and developmental disability, and may be considered as an alternative if required.
If other antipsychotic drugs are considered for ‘off label’ use to manage challenging behaviour in children or adults with developmental disability, they should be started by a clinician with expertise in using psychotropic drugs (eg child psychiatrist, paediatrician or general practitioner with expertise, psychiatrist).
Evidence is lacking to support the use of anticonvulsants for challenging behaviour in children and adults with developmental disability.
NB1: Nondrug interventions include psychological, social, functional and environmental interventions; see Behaviour support for a person with developmental disability.
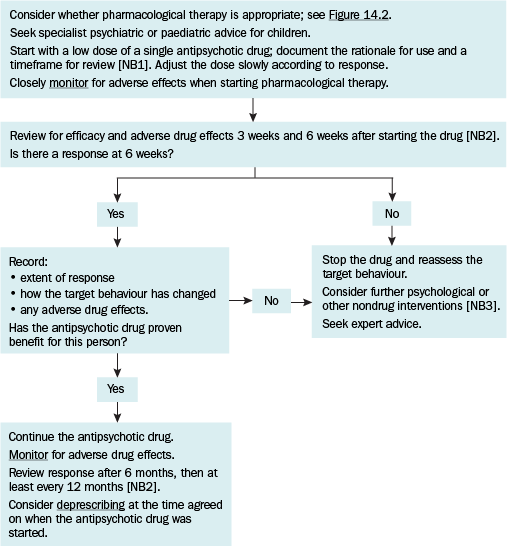
NB1: Clearly communicate to the person, or their substitute decision maker if they lack capacity, a timeframe for review to assess response, and to consider stopping the drug.
NB2: Review response earlier if needed.
NB3: Nondrug interventions include psychological, social, functional and environmental interventions; see Behaviour support for a person with developmental disability.
Deprescribing antipsychotics for challenging behaviour
Over-medication of people with intellectual disability has been reported locally and internationally and remains a source of great concern to government and non-government bodies, patients and caregivers. Stopping antipsychotics used for challenging behaviour in a person with developmental disability can improve cognitive function and increase their time spent engaged in activity; however, it may be associated with worsening behaviour and withdrawal effects (eg increased incidence of tardive dyskinesia).
Deprescribing may be considered in people who have successfully responded to a positive behaviour support plan; seek specialist advice (eg paediatrician, psychiatrist) to deprescribe antipsychotics in people who initially had severe challenging behaviour. Factors that predict successful withdrawal include a lower baseline antipsychotic dose and not previously failing trials of discontinuation. Consider reasonable adjustments needed to accommodate communication or cognitive difficulty.
Before deprescribing an antipsychotic for challenging behaviour, discuss the process with the person and their parents or carers, considering the:
- agreed goals of care and preferences of the person, parents or carers
- process for withdrawal
- fears, concerns and expectations of the person and their parents or carers about deprescribing
- benefits of deprescribing (eg reduced adverse effects) versus potential harms (eg worsening behaviour, withdrawal effects).
There is limited evidence to support a specific protocol for deprescribing antipsychotic drugs used for challenging behaviour in people with developmental disability. To reduce the risk of behaviour worsening:
- ensure the behaviour support plan is maintained
- avoid attempting withdrawal during a stressful period (eg transition of care)
- withdraw one drug at a time
- decrease the dose of the drug slowly (10 to 25% reduction per month or slower)
- allow time (ie weeks) to monitor effects between each dose reduction
- monitor for and document beneficial and adverse effects of deprescribing; advise the person and their parents or carers about common adverse effects of stopping or reducing the dose of antipsychotics (see Common adverse effects of stopping or reducing the dose of an antipsychotic).
Make and document a plan for withdrawal of an antipsychotic drug for challenging behaviour with the person and their parents or carers. Establish a baseline of behaviour and monitor daily throughout the drug withdrawal process. Include the approach to monitoring, dosage adjustment, and behavioural interventions if the target behaviour remerges—record relevant information in the person’s behaviour support plan. Engage parents or carers as partners in monitoring response to decreasing dosage.
