Fatigue: overview
Fatigue is a subjective experience that everyone can identify with, and a challenging problem in primary care. It is one of the most frequent reasons for presentation in general practiceFinley, 2018. The population prevalence of fatigue has been found to be as high as 20% in adultsGalland-Decker, 2019, but this could be an underestimate because fatigue may be unreported, especially when it occurs with other symptoms that are easier to describeHarrison, 2008. Fatigue is often distressing for patients and may impact significantly on activities of daily living.
It is often difficult to precisely convey the experience of fatigue to others, as it means something different to everyone. Fatigue has been defined as an enduring feeling of tiredness, where the constant subjective sensation of weariness is usually not relieved by restMayo Clinic Staff, 2020MedlinePlus, Accessed Mar 2022. Patients and their families, however, may use a variety of terms to describe fatigue including ‘tiredness’, ‘weakness’, ‘sluggishness’, ‘sleepiness’, ‘feeling flat’ or ‘lethargic’. It is important to endeavour to understand what the patient means (ie exactly what they are experiencing); see History and examination in fatigue.
The onset of fatigue may be acute or insidious, and patients may attribute it to a discrete event. Patients may also present with worsening of pre-existing fatigue. The causes of and contributors to fatigue are broad and include underlying disease and psychological, social and behavioural factors; in most cases, several of these factors coexist. The pathophysiology of fatigue is poorly understoodAlexander, 2010. Fatigue may resolve spontaneously or after the precipitating factor (eg acute illness) has resolved; however, especially when fatigue persists, a wide range of associated conditions must be consideredGodwin, 1999; see Conditions commonly associated with fatigue.
For key points to consider when patients present with fatigue, see Key points to consider when patients present with fatigue.
- Fatigue may be related to many identifiable biopsychosocial factors; however, it is often unexplained or inadequately explained.
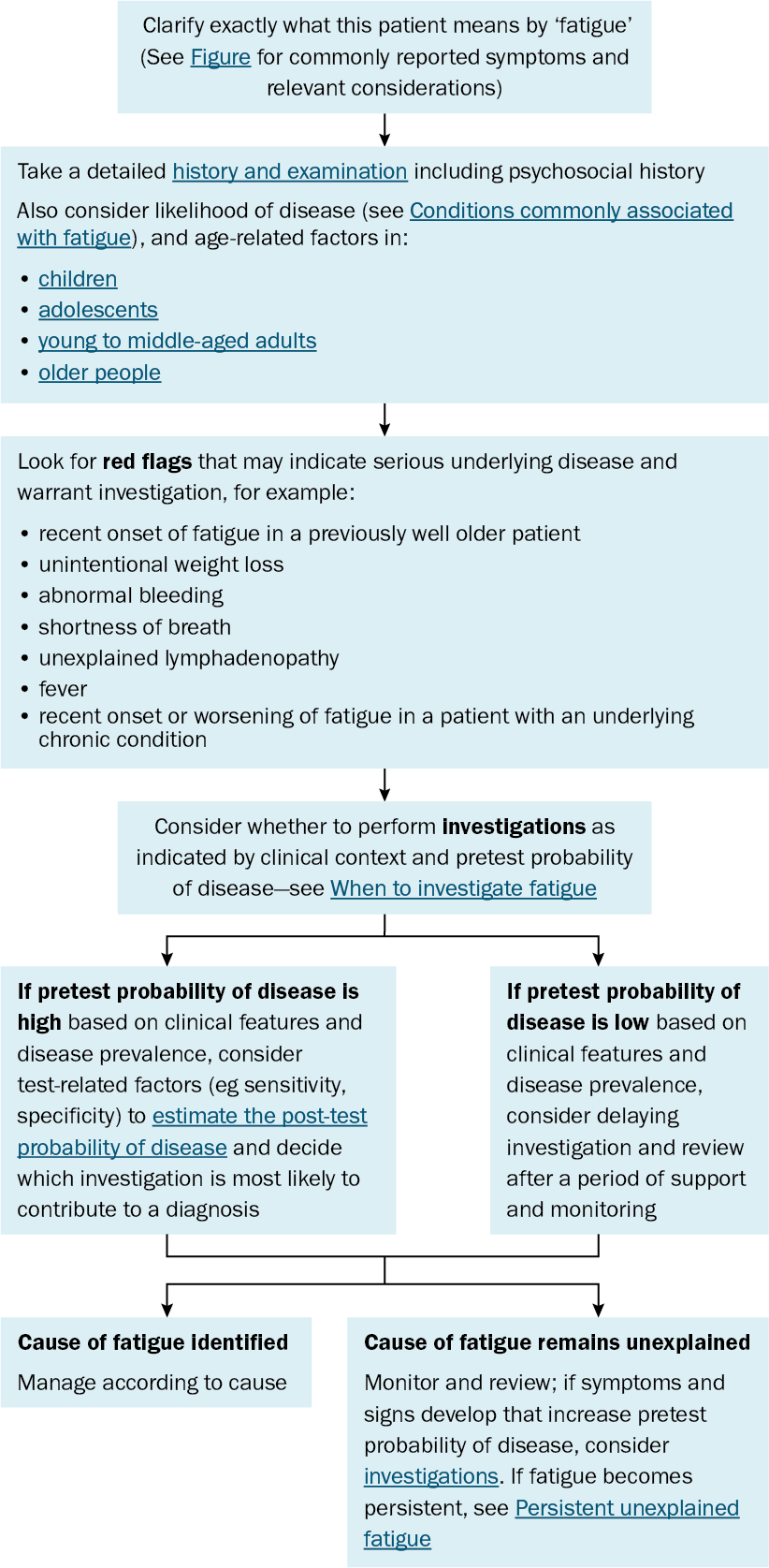
- The diagnostic approach starts with thorough clinical assessment, which includes listening carefully to patient accounts, taking a history and physical examination.
- Familiarity with conditions that are commonly associated with fatigue and their likelihood in a particular patient group will help guide management.
- As most patients with fatigue do not have relevant abnormal pathology test results, investigations should be used selectively as guided by history and clinical examination.
The diagnostic approach to a patient presenting with fatigue is outlined in Diagnostic process for a patient presenting with fatigue.