Summary of menopause management
The goals of managing menopause are to alleviate symptoms and reduce the risk of osteoporosis.
Options for managing menopause include systemic menopausal hormone therapies (MHT), intravaginal estrogen therapy, and nonhormonal therapies.
Systemic MHT is the most effective treatment for vasomotor symptoms (hot flushes and night sweats), and can also aid sleep. It also plays an important role in prevention and management of osteoporosis. Systemic MHT includes:
- estrogen-only MHT
- combined MHT (estrogen plus progestogen) in a cyclical combined or continuous combined regimen (progestogen must be added to systemic estrogen in individuals with endometrial tissue)
- other forms of systemic MHT—tibolone and conjugated estrogens+bazedoxifene (these are not suitable for perimenopausal individuals).
Intravaginal estrogen therapy is the most effective therapy for symptoms of vulvovaginal atrophy. It can also reduce the risk of recurrent urinary tract infections and improve some urinary symptoms (including urinary urge incontinence).
Nonhormonal therapies include drug and nondrug approaches, such as:
- nonhormonal drug therapy for vasomotor symptoms, which can also help sleep, mood disturbance and neuropathic pain
- nondrug therapy for vasomotor symptoms, including cognitive behavioural therapy
- nonhormonal therapy for urinary symptoms (eg stress and urge incontinence)
- nonhormonal vaginal therapy for vaginal dryness.
To reduce the risk of osteoporosis, use systemic MHT for perimenopausal or postmenopausal individuals with low bone mineral density, and individuals with premature ovarian insufficiency (POI) or early menopause, regardless of bone mineral density. For detailed advice, see Osteoporosis and minimal-trauma fracture and Other drugs for osteoporosis.
For a summary of the approach to starting therapy for menopause, see Approach to starting therapy for menopause.
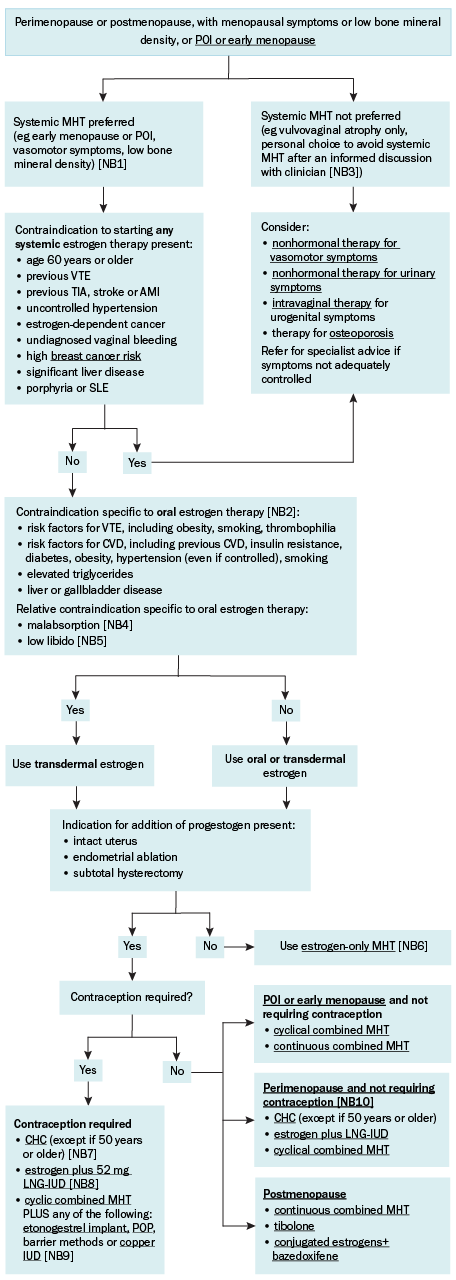
AMI = acute myocardial infarction; CHC = combined hormonal contraception; CVD = cardiovascular disease; LNG-IUD = levonorgestrel-releasing intrauterine contraceptive device; MHT = menopausal hormone therapy; POI = premature ovarian insufficiency; POP = progestogen-only contraceptive pill; SLE = systemic lupus erythematosus; SNRI = serotonin noradrenaline reuptake inhibitor; SSRI = selective serotonin reuptake inhibitor; TIA = transient ischaemic attack VTE = venous thromboembolism
NB1: Consider benefits and harms of systemic menopausal hormone therapy before prescribing. See also Systemic MHT in specific patient groups.
NB2: If the patient has any contraindications to oral estrogen, transdermal estrogen can be used. Oral estrogen or other forms of systemic MHT (tibolone or conjugated estrogens+bazedoxifene) should only be used with advice from a specialist.
NB3: If the individual has POI or early menopause, systemic MHT is strongly recommended to prevent cardiovascular disease and osteoporosis, regardless of menopausal symptoms or bone mineral density.
NB4: Malabsorption is a relative contraindication because it may result in breakthrough bleeding or inadequate symptom relief. Transdermal estrogen is preferred to avoid these complications; the contraceptive vaginal ring is an alternative for individuals younger than 50 years.
NB5: Low libido is a relative contraindication; oral estrogen increases sex hormone–binding globulin, which reduces bioavailable testosterone and may exacerbate low libido; this effect is also seen with use of the contraceptive vaginal ring. Transdermal estrogen is preferred to avoid this.
NB6: Addition of a progestogen may be required in individuals with significant endometriosis to prevent stimulation of endometrial deposits and malignant transformation (even if they have had a total hysterectomy); seek specialist advice.
NB7: For individuals with POI, CHC must be used continuously (no hormone-free intervals).
NB8: Contraceptive methods other than the 52 mg LNG-IUD cannot be used for endometrial protection in combination with estrogen-only MHT because evidence is lacking for a suppressive effect on estrogen-driven endometrial hyperplasia.
NB9: Although data are lacking on concurrent use for contraception, expert consensus is that the etonogestrel implant, POP and copper IUD can be combined with cyclical combined MHT. Heavy bleeding associated with use of the copper IUD may limit its use in some perimenopausal patients. The efficacy of barrier methods is not affected by the use of MHT.
NB10: CHC and LNG-IUD are being used for hormone replacement rather than for contraception.
General advice on managing symptoms that may develop or be exacerbated in menopause is available in the following topics:
- Low libido in females
- Sexual pain in females
- Orgasm difficulties in females
- Anxiety disorders and depression—perimenopausal individuals are particularly at risk of depression. Nonhormonal drug therapy for vasomotor symptoms outlines the efficacy of some antidepressants in reducing vasomotor symptoms and sleep disturbance, which may aid choice of drug for managing depression.
Midlife is an appropriate time to assess and screen for age-related health conditions. A general health check is recommended in any individual seeking medical advice about menopause. Screening for cardiovascular disease risk is recommended in all adults aged 45 years and older, people with diabetes aged 35 years and older and First Nations peoples aged 30 years and older. In addition to assessing standard cardiovascular risk factors, consider additional female-specific risk factors:
- pregnancy-related factors (eg pre-eclampsia, gestational diabetes)
- polycystic ovary syndrome
- breast cancer therapy
- POI and early menopause.
In individuals with POI or early menopause, systemic MHT is beneficial for primary prevention of cardiovascular disease; evidence that systemic MHT has a role in cardiovascular disease prevention outside this group is insufficient.
Patient information sheets on lifestyle change are available from the Australian Menopause Society website. See also the Royal Australian College of General Practitioners (RACGP) Guidelines for preventive activities in general practice for advice on a midlife health checkup.
Compounded and complementary medicines are generally not recommended for treatment of menopause because they have not been shown to be safe and effective; see Compounded and complementary medicines for menopause for more information.
