Overview of diagnosis of male androgen deficiency
Approach to diagnosis in suspected male androgen deficiency outlines an approach to diagnosis in suspected androgen deficiency. The aims are to:
- determine whether criteria for androgen deficiency are met
- exclude differential diagnoses
- undertake initial investigations to seek the cause of androgen deficiency (if feasible) before referral.
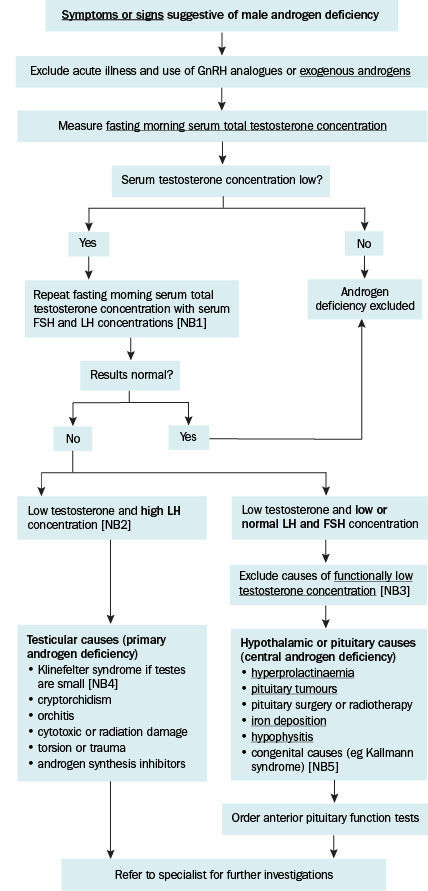
FSH = follicle stimulating hormone; GnRH = gonadotrophin-releasing hormone; LH = luteinising hormone
NB1: Serum FSH concentration may be easier to interpret than LH, as LH is pulsatile. Serum FSH concentration is also part of assessment for male infertility, which can accompany some causes of androgen deficiency.
NB2: Low testosterone and slightly elevated LH concentrations may be due to normal ageing; see Interpreting serum testosterone concentrations..
NB3: Mildly low testosterone and normal LH concentrations may be due to comorbidities such as obesity, diabetes, depression, or use of opioids, high-dose corticosteroids, alcohol or marijuana; see Interpreting serum testosterone concentrations.
NB4: For information on Klinefelter syndrome, see the US National Library of Medicine Medline Plus website.
NB5: For information on Kallmann syndrome, see the US National Library of Medicine Medline Plus website.
