Assessment for peripheral neuropathy
Introduction
Peripheral neuropathy is one of the major contributors to foot wounds. Peripheral neuropathy can involve damage to:
- sensory nerves, causing reduced temperature, touch and pain sensation
- motor nerves, causing foot deformity from altered foot biomechanics
- autonomic nerves, causing reduced skin quality and changes to peripheral vascular function.
See Causes, classification and types of peripheral neuropathy for a comprehensive list of causes of peripheral neuropathy.
For management of patients found to have peripheral neuropathy, see Interventions for wounds on a high-risk foot.
10 gram monofilament test
A calibrated 10 gram monofilament is an objective, simple instrument used to screen the foot for loss of protective sensation. There is disagreement in the literature about the accuracy and method of application of this test. This test should be considered in conjunction with the overall neurological examination and clinical review.
The process for sensory examination using a calibrated 10 gram monofilament is:
- Perform in a quiet and relaxed setting.
- Demonstrate buckling of the 10 gram monofilament on the patient's hand so they know what to expect.
- Position the patient so they can't see when and where the monofilament is applied, or ask them to close their eyes.
- Ask the patient to tell you if they feel the monofilament, and where they feel it (left or right foot).
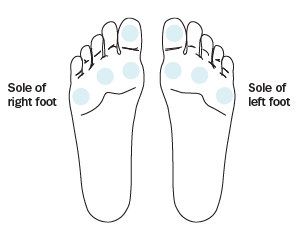
- Apply the monofilament perpendicular to the skin surface to at least four sites on each foot (see Peripheral neuropathy testing sites on the sole of the foot). Do not put the monofilament on a wound, callus, scar or necrotic tissue. Do not let the monofilament slide across the skin or make repetitive contact at the test site. Each site can be tested up to three times if the patient does not respond.
- Apply sufficient force to make the monofilament bend or buckle (see Screening using a 10 gram monofilament). When the monofilament bends, its tip is exerting a pressure of 10 grams.
- The total time taken to touch the skin, make contact, and remove the monofilament should be approximately 2 to 3 seconds.

If a patient cannot detect the pressure of the monofilament at any one of the sites, this may indicate peripheral neuropathy and loss of protective sensation1. For patients with suspected peripheral neuropathy, undertake a neurological exam for further assessment.
If the patient can detect the monofilament at all sites, they have adequate sensation. Consider an alternative cause for the wound (eg peripheral arterial disease).
It is important to use a properly calibrated monofilament so that 10 grams of linear pressure is applied. For practice points about care of a monofilament, see Practice points for care of a monofilament. Clinics screening more than 10 patients per day require more than one 10 gram monofilament.
- if a monofilament is bent or damaged, replace it
- if used daily, replace monofilament every 6 months
- if used less than daily, replace monofilament every 12 months
- disposable monofilaments are preferred
Ipswich touch test
If a calibrated 10 gram monofilament isn't available, the Ipswich touch test may be used. The Ipswich touch test is conducted by lightly touching the first, third, and fifth toes, and the dorsum of the hallux, for 1 to 2 seconds. The patient has their eyes shut and announces if they feel the touch. If they cannot feel the touch at any of the sites, this strongly suggests sensory neuropathy.
