Introduction
If ulcers or wounds become infected, healing can be delayed. Although ulcers can occur due to a primary infectious disease, more often ulcers with a noninfectious cause develop a secondary infection.
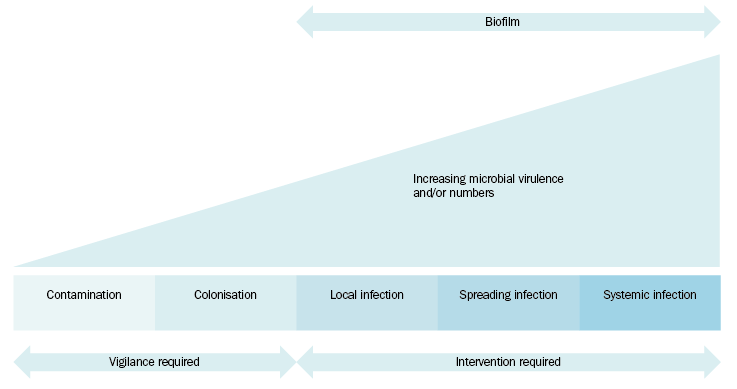
The wound infection continuum is a guide for when to initiate topical and systemic antimicrobial management strategies (see The wound infection continuum). Signs and symptoms of each stage of wound infection are provided in #lwg2-c18-s2-1__tlwg2-c18-tbl2.
Do not use systemic antimicrobials unless the wound is clinically infected.
Redness on a patient's leg is commonly misdiagnosed as cellulitis—consider differential diagnoses; see Common causes of a red leg.
- venous dermatitis
- allergic contact dermatitis (eg from a dressing)
- irritant contact dermatitis (eg from exudate or the dressing)
- other dermatitis
- superficial thrombophlebitis
- cellulitis
- superficial fungal infections
- cutaneous drug reaction
- erythema nodosum
- erythromelalgia
All chronic wounds are contaminated either by transient or commensal micro-organisms that live on the skin or have been introduced (eg during injury). Routine use of topical antiseptics, antibiotics or antimicrobial dressings for healing ulcers or wounds is not recommended. However, when clinical infection occurs, intervention may be warranted.
Signs of local wound infection can be covert or overt (see #lwg2-c18-s2-1__tlwg2-c18-tbl2). Covert (subtle) signs of infection can develop into overt signs of infection (see The wound infection continuum). Use antiseptics for local infection (eg polyhexamethylene biguanide [PHMB], octenidine dihydrochloride, chlorhexidine, povidone-iodine). Chlorhexidine and povidone-iodine must be washed off after 5 minutes to avoid cytotoxicity; see Cleansing and debridement.
For spreading or systemic infection, systemic antibiotics in addition to topical management strategies are recommended (see Systemic antimicrobial therapy). Debridement (if not contraindicated) should be undertaken in combination with antibiotics to disrupt biofilm and impair reformation. Appropriate surgical intervention is important in management of deep soft tissue infections for source control.
The practice of using antibiotic therapy alone to promote healing by decreasing bacterial burden is not recommended. A combination of debridement, wound cleansing and appropriate dressing selection is essential (see Ulcer and wound dressings).
