Diagnosis of oral and oropharyngeal infection caused by Candida and related species
Diagnosis of infection caused by Candida and related species (oral and oropharyngeal candidiasis) is based on the clinical presentation and assessment of risk factors; many people are asymptomatic. If present, symptoms include an unpleasant taste, loss of taste or, in some cases, a burning pain while eating.
On examination, oral and oropharyngeal candidiasis present as eitherNg, 2013:
- pseudomembranous – creamy white curd, papules and plaques that can be peeled off (on the mucosa, palate, tongue or pharynx – see Pseudomembranous candidiasis for a photo)
- erythematous – erythema without plaques affecting the palate and tongue; the tongue may appear depapillated and smooth (see Erythematous candidiasis for a photo).
If any ‘red flag’ features of oral mucosal disease are present, refer to a specialist.
Chronic hyperplastic candidiasis is often asymptomatic and presents as nonremovable white plaques that may appear nodular. It may resemble oral leukoplakia or oral cancer (see Chronic hyperplastic candidiasis for a photo). Refer patients to a specialist for biopsy and management1.
Painful erythema and fissuring of the corners of the mouth can also be a sign of candidiasis – see Angular cheilitis for further information.
For adults with oropharyngeal candidiasis who have oesophageal symptoms (eg swallowing difficulties), consider oesophageal candidiasis.
Chronic oral or oropharyngeal candidiasis is an indicator condition for HIV testing2; offer HIV testing, regardless of whether the patient has behavioural or epidemiological risk factors for HIV infection.
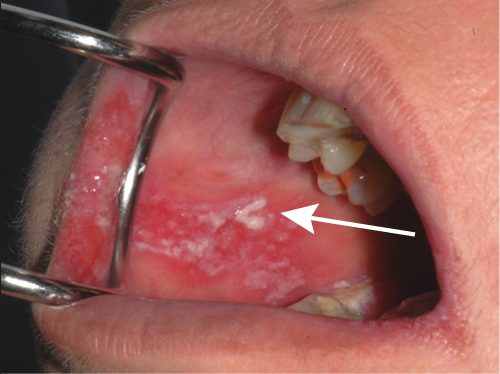
Photo sourced with permission from Associate Professor Sue-Ching Yeoh.
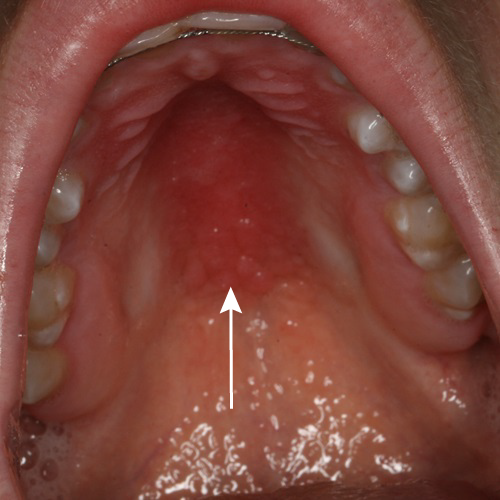
Photo sourced with permission from Associate Professor Sue-Ching Yeoh.
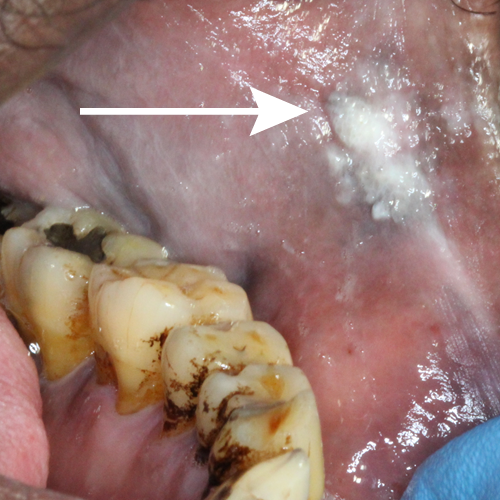
Photo sourced with permission from Associate Professor Sue-Ching Yeoh.
