Principles of management of NSTEACS
Patients with acute myocardial ischaemia without persistent ST elevation on their presenting electrocardiogram (ECG) are diagnosed as having a non–ST elevation acute coronary syndrome (NSTEACS). NSTEACS is further divided into 2 groups based on cardiac troponin values:
- non–ST elevation myocardial infarction (NSTEMI), defined by elevated troponin
- unstable angina, defined as myocardial ischaemia at rest or on minimal exertion in the absence of acute cardiomyocyte necrosis (ie normal troponin levels); unstable angina has become a less common diagnosis because of the introduction of high-sensitivity troponin assays that can detect minimal amounts of myocardial necrosis.
The recommendations in this topic refer to Type 1 myocardial infarction; Type 2 myocardial infarction should be treated according to the cause. See Classification of coronary ischaemic syndromes for information on Type 1 and Type 2 myocardial infarctions.
For patients with confirmed NSTEACS, management involves risk stratification to determine whether and when to use an invasive management (ie coronary angiography and revascularisation). Unlike ST elevation myocardial infarction (STEMI), thrombolytic therapy is not an option for NSTEACS.
Drug therapy for NSTEACS can include dual antiplatelet therapy, parenteral anticoagulant therapy and in some cases, glycoprotein IIb/IIIa inhibitors.
Following NSTEACS, most patients benefit from long-term combination therapy with an antiplatelet drug, a statin, an angiotensin converting enzyme inhibitor (ACEI) (or angiotensin II receptor blocker [ARB]) and a beta blocker; see Long-term management of acute coronary syndromes.
See Overview of management of non-ST elevation acute coronary syndrome (NSTEACS) for an overview of the management of NSTEACS.
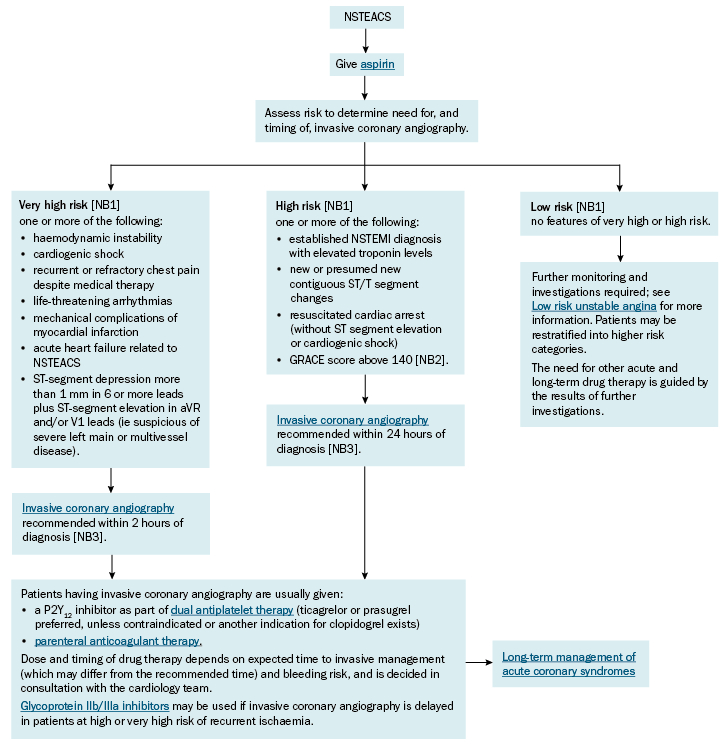
GRACE = Global Registry of Acute Coronary Events; NSTEACS = non–ST elevation acute coronary syndrome; NSTEMI = non–ST elevation myocardial infarction
NB1: These features are general determinants of risk. Risk stratification is a clinically determined decision, and these categories may not be an absolute or a true reflection of the individual patient’s risk.
NB2: An online calculator for the GRACE score can be found on the MD+CALC website.
NB3: Every effort should be made to meet these recommended timeframes; however, if these timeframes are not feasible, aim for invasive management as early as possible. Thrombolytic therapy is not an option for NSTEACS, including if the recommended timeframes for invasive management cannot be met.
