Stepwise management of stable COPD
Management of stable chronic obstructive pulmonary disease (COPD) follows a stepwise escalation of nondrug and drug interventions, introduced according to disease severity, as outlined in Management pathway for stable COPD.
Discuss the following short- and long-term goals of managing stable COPD with patients:
- reducing symptoms
- reducing frequency and severity of exacerbations
- improving exercise tolerance
- improving health-related quality of life
- slowing disease progression.
All patients with COPD can benefit from general measures, including:
- smoking cessation—this is the single most important intervention to prevent or limit lung damage in COPD
- physical activity
- pulmonary rehabilitation (for symptomatic patients)
- maintenance of up-to-date vaccination
- good nutrition.
For patients with few symptoms and a COPD Assessment Test (CAT) score less than 10, these general measures may be adequate initially.
As the disease progresses, drug therapy can be introduced. Drug therapy relieves symptoms, improves quality of life and reduces the frequency of exacerbations. The effect of drug treatment on mortality remains unclear. Drug therapy is typically introduced sequentially as follows:
- short-acting bronchodilator therapy—usually a short-acting beta2 agonist (SABA)
- long-acting bronchodilator monotherapy—a long-acting beta2 agonist (LABA) or long-acting muscarinic antagonist (LAMA)
- long-acting bronchodilator dual therapy—LABA plus LAMA combination therapy
- LABA, LAMA plus inhaled corticosteroid triple therapy.
Other treatments used infrequently include mucolytics, antibiotics and theophylline. Oxygen, noninvasive ventilation and surgical or interventional procedures can be considered for severe disease.
Review drug therapy 3 to 6 months after starting or adjusting therapy and regularly thereafter to assess response and tolerability. Check inhaler technique and adherence at each visit, and before considering stepping up therapy; up to 90% of patients use their devices incorrectly.
Nondrug measures that can provide symptomatic relief of dyspnoea include handheld fans, pursed-lip breathing, and breathlessness recovery positions (eg leaning forward).
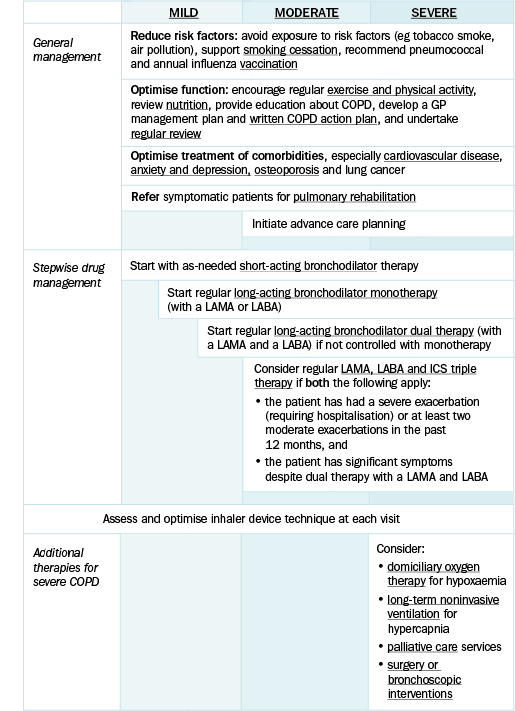
COPD = chronic obstructive pulmonary disease; GP = general practitioner; ICS = inhaled corticosteroids; LABA = long-acting beta2 agonist; LAMA = long-acting muscarinic antagonist
Adapted with permission from Yang I, Brown JL, George J, Jenkins S, McDonald C, McDonald CF, McDonald V, et al. The COPD-X Plan: Australian and New Zealand Guidelines for the management of chronic obstructive pulmonary disease 2020, version 2.61. Brisbane, QLD: Lung Foundation Australia; February 2020. [URL]
Printable figure available from the Lung Foundation Australia website.
Effective management of COPD should involve a multidisciplinary team including nursing and allied health professionals. The general practitioner is usually best suited to coordinate management. Multidisciplinary care for COPD outlines the common professions included in a multidisciplinary team for COPD.
A multidisciplinary team to manage COPD can include:
- GP to manage drug therapy and regular reviews, to develop a management plan [NB1] and to coordinate overall care
- respiratory physician to manage advanced COPD, confirm the diagnosis, exclude complicating factors and help develop a self-management plan in complex patients
- practice nurse or respiratory educator to perform spirometry testing, assess and educate patients on inhaler technique and adherence, and provide training in self-management
- respiratory nurse to assess the need for and arrange specialist treatments such as domiciliary oxygen therapy and noninvasive ventilation
- pulmonary rehabilitation clinic
- physiotherapist to provide exercise training and pulmonary rehabilitation, including teaching airway clearance techniques
- occupational therapist to assess ability to perform daily tasks of living, and arrange home modifications and adaptive equipment
- speech therapist to provide swallowing training to avoid aspiration
- psychologist or psychiatrist to manage psychiatric disorders (eg anxiety, depression), which are common comorbidities of COPD
- pharmacist to provide medication advice, opportunistic assessment, home medication review and education on inhaler technique and adherence
- dietician to provide advice about nutrition
- council- or government-supported programs to assist with daily tasks of living (eg home visits to assist with showering or cleaning)
- other services including hospital-in-the-home, early discharge schemes and palliative care services.
COPD = chronic obstructive pulmonary disease; GP = general practitioner
NB1: Subsidised allied health services may be available through a pulmonary rehabilitation program or a GP management plan.
